DIABETIC VITRECTOMY/TRD BASICS
Indications for surgery
Pre- and post-surgical considerations
Intraoperative considerations
Surgical Steps
Diabetic vitrectomy/TRD basics
Back to topIndications for surgery
Vitreous hemorrhage
- Vitreous hemorrhage can clear spontaneously and a PPV will decrease the longevity of intravitreal anti-VEGF agents in the future, so some surgeons prefer to observe initially. A combination of anti-VEGF agents and laser to visible retina in clinic can aid in hemorrhage clearance.
- However, if there are large amounts of neovascularization, the utilization of anti-VEGF agents or laser can lead to fibrosis, the creation or worsening of an underlying tractional retinal detachment, or the “crunch” phenomenon.
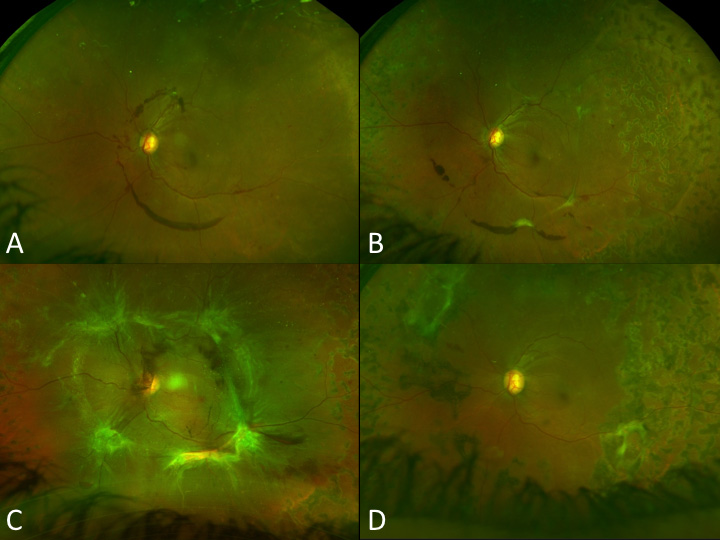
Figure 1: A patient presents with proliferative diabetic retinopathy, treated with serial panretinal photocoagulation with early tenting of the neovascularization. (A, B) Eventually this progressed through the crunch phenomenon to create a combined tractional retinal detachment and rhegmatogenous detachment requiring surgery. (C, D) Image Credit: Thanos Papakostas
- Factors which can lead to earlier intervention for vitreous hemorrhage include:
- Underlying pathology, including: the development of or progression of a known underlying tractional retinal detachment with or without a rhegmatogenous component, vitreomacular traction or worsening epiretinal membrane, or the possibility of anterior hyaloidal proliferation, especially in cases of recurrent hemorrhage treated with adequate panretinal photocoagulation in the past.
- Neovascularization of the iris (NVI) or angle (NVA) can cause increased intraocular pressure. The presence of NVA and/or NVI is linked to a decreased chance of spontaneous hemorrhage clearance.
- Vitreous hemorrhage in a functionally or truly monocular patient.
- Vitreous hemorrhage in a patient who has not been treated with prior laser.
Tractional retinal detachment
- In extramacular tractional retinal detachments, surgeons may choose to observe cautiously, with the expectation of surgery if the detachment progresses or involves the macula. This is particularly true in young patients where hyaloidal separation is unlikely and an increased risk of retinal breaks exist with surgery.
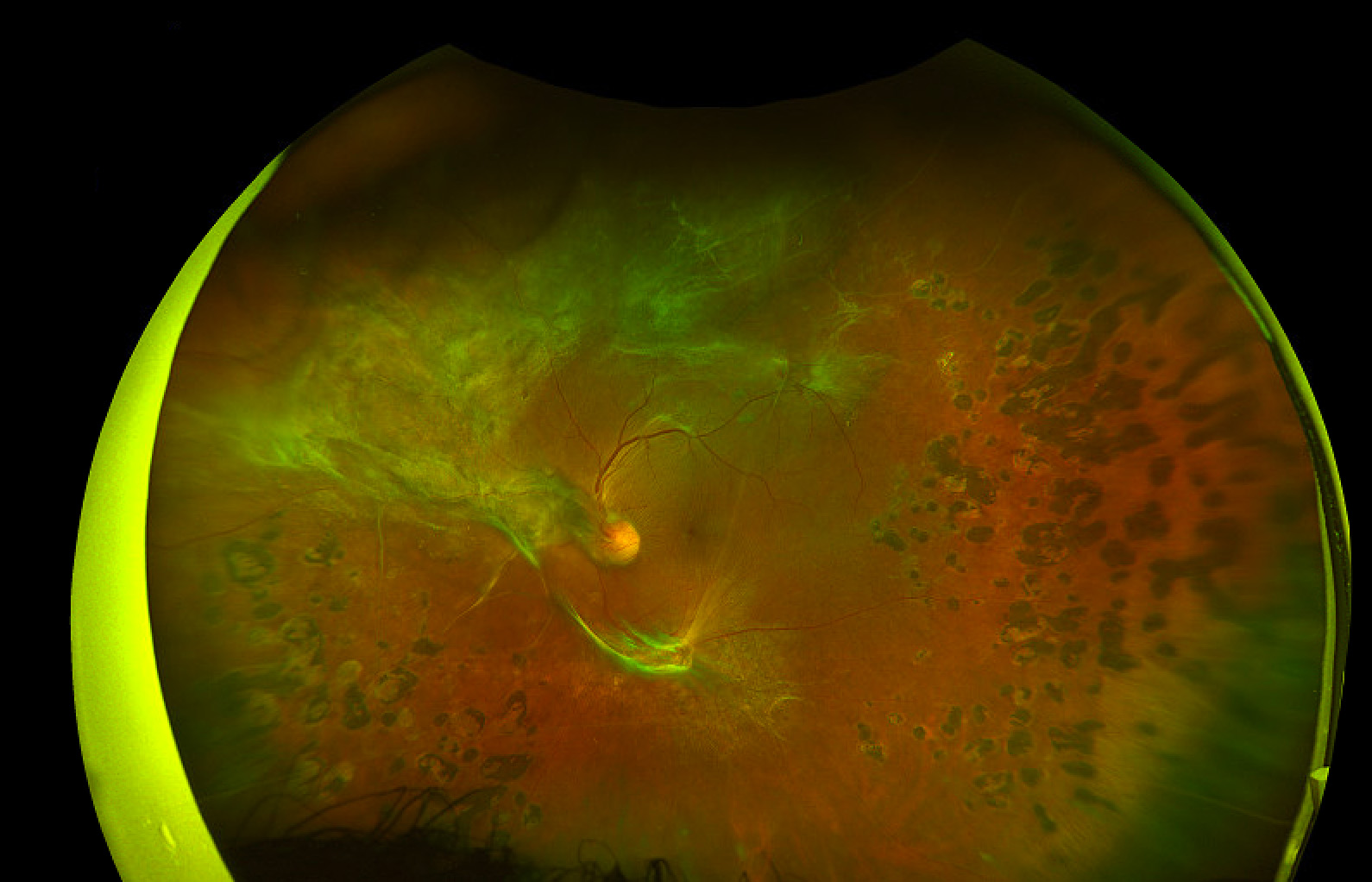
Figure 2: A 43-year-old female presents with a TRD encroaching on her macula. OCT showed no macular subretinal fluid. Given her young age and hyaloid status, the decision was made to monitor closely with small additional sessions of panretinal photocoagulation. Image Credit: Sruthi Arepalli
- In functionally monocular patients, progression of a tractional retinal detachment, even outside of the macula may prompt intervention.
Combined tractional and rhegmatogenous detachment
- The same processes leading to the formation of a tractional retinal detachment can also cause a combined tractional and rhegmatogenous detachment with retinal breaks forming in locations different than a typical retinal detachment. These include posterior breaks, as well as breaks along areas of traction or vessels.
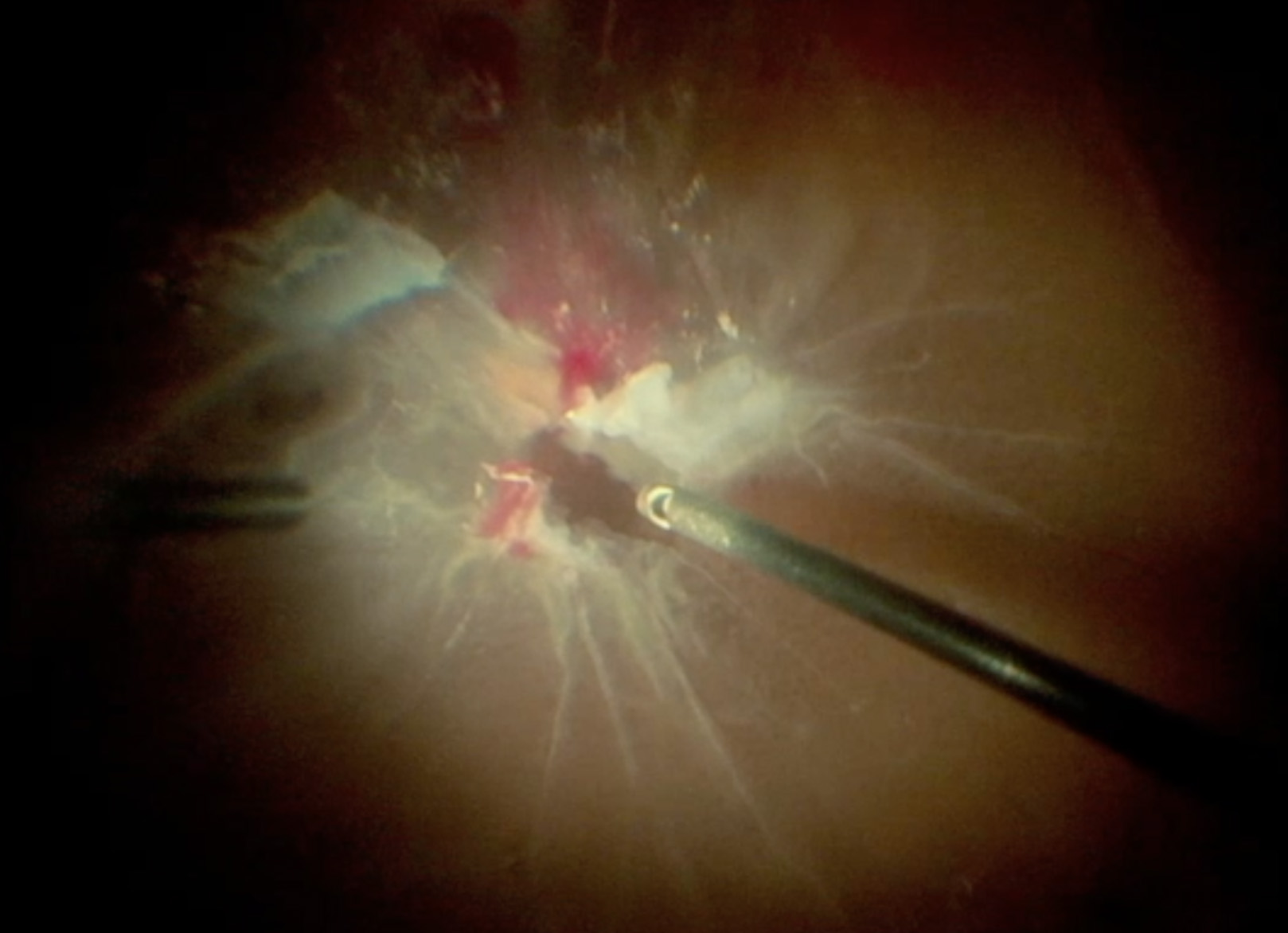
Figure 3: A combined TRD and RRD reveals a posterior break superior to the nerve. In combined tractional and rhegmatogenous detachments, breaks may appear more posteriorly than in a sole rhegmatogenous detachment. Image Credit: Thanos Papakostas
Vitreomacular traction and epiretinal membrane
- In cases of foveal distortion and edema in the setting of diabetic retinopathy, patients can be trialed with anti-VEGF. If this fails to improve symptoms, surgery can remove these the traction on the retinal surface. In cases of especially taut or dense fibrovascular proliferations, surgeons may want to avoid pre-operative anti-VEGF as this may predispose the patient to developing the “crunch” phenomenon.
Pre- and post-surgical considerations
Systemic manifestations of diabetes
- Often, patients with proliferative diabetic retinopathy have systemic complications of the disease. These include cardiovascular issues and renal compromise requiring dialysis, which may limit surgical clearance as well as the patient’s ability to adhere to pre and post-operative care. Further, the renal dysfunction can limit the types of drugs used in the post-operative period, such as acetazolamide.
- Management of blood sugars and other co-morbidities with the primary care doctor prior to surgery is important in order to maximize the chances of surgical clearance.
Visual potential
- Pre-operative imaging is useful to council patients on visual expectations. OCT findings such as the disorganization of retinal layers, retinal thinning, and/or ellipsoidal zone attenuation portend a worse visual prognosis. Pre-operative fluorescein angiography or optical coherence tomography angiography can assess for macular ischemia, another risk factor for poor visual outcomes.
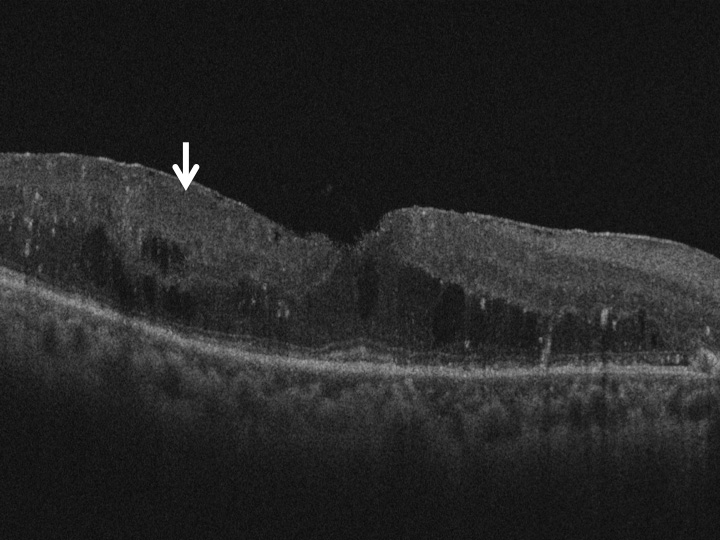
Figure 4: Disorganization of the retinal layers, particularly the inner retinal layers, as denoted by the white arrow has been linked to worse visual outcomes. Image Credit: Sruthi Arepalli
Pre-operative anti-VEGF
- Some physicians prefer to administer anti-VEGF therapy prior to surgery, with a range of 1-10 days before being the most common timeframe. Some have shown better visual and surgical outcomes when anti-VEGF is given 5-10 days before to surgery rather than immediately prior. Physicians may prefer to administer multiple rounds of anti-VEGF prior to surgery. Anti-VEGF can decrease intraoperative bleeding and improve surgical plane delineation. Unfortunately, pre-operative anti-VEGF can also accelerate tractional detachment formation, otherwise known as the “crunch” phenomenon. It can also hide intraoperative bleeding which may become pronounced in the post-operative period. Caution should be exercised when administering anti-VEGF to those with fibrovascular proliferation or tractional detachments adjacent to the macula as these can progress quickly in the setting of ant-VEGF.
Pre-operative laser
- Some providers also prefer to place panretinal photocoagulation prior to surgical intervention. This can help regress neovascularization and provide more stability when peeling and segmenting fibrovascular proliferations. The “crunch” phenomenon can also occur after panretinal photocoagulation, so caution should be applied with membranes adjacent to the macula and the sessions can be broken up into smaller subsets.
Lens status
- There are situations where the view may be compromised from lens changes or anterior hyaloidal proliferation is suspected. In these cases, a cataract surgery, either staged or in combination with a vitrectomy should be considered. If phacoemulsification cannot be done before or during the time of vitrectomy, a pars plana lensectomy may be required. Since the removal of the lens increases the risk of anterior neovascularization, many surgeons will opt to keep the lens if possible. Concurrent phacoemulsification may create corneal edema making dissection of membranes and complex surgical procedures difficult.
Intraoperative considerations
Which gauge?
- Surgeon preference includes 23, 25 or 27 gauge systems, or a combination (I.e., using large gauge ports with a smaller gauge cutter to dissect and segment fibrovascular proliferation).
Diabetic TRD
Video credit: Thanos Papakostas; Editing and Narration: Sruthi Arepalli
What’s in the bottle?
- If the patient is phakic, surgeons can add in dextrose (3 mL of dextrose 50%). This helps prevent lens opacification during surgery and afterwards. Some also prefer epinephrine (preservative free 0.3 mL of 1:1000 epinephrine) to help with dilation and control intraoperative bleeding, but this may mask hemorrhage that presents post-operatively.
Visualization
- When working posteriorly, a contact lens or high magnification viewing system is preferred. When working peripherally, a wide angle viewing system is best.
Surgical Steps
Peripheral vitrectomy
- Unlike with rhegmatogenous detachments, it is unusual to have a complete posterior vitreous detachment in a tractional retinal detachment. The vitreous may be released in the mid-periphery but is usually attached posteriorly.
- When approaching the vitreous, remove the vitreous from the two superior ports to avoid vitreous incarceration and peripheral retinal tears.
- After clearing the vitreous from these ports, remove the vitreous from behind the lens, while taking care to spare the posterior capsule. If the hemorrhage cannot be cleared well enough in a phakic eye, a lensectomy may be necessary. If it cannot be cleared in a pseudophakic patient, a capsulotomy may be required.
Clearing Vitreous Hemorrhage
Video credit: Sruthi Arepalli
- If the mid-peripheral vitreous is elevated, incise the hyaloid and extend this opening 360 degrees to release the anterior-posterior traction and separate the retina from the hyaloid. Remove the anterior vitreous. At this point, clotted vitreous blood in the peripheral retina can carefully be removed with scleral depression, or this can be left for the end of the case. Some surgeons prefer to leave this scleral depression for the end of the case as the intraocular pressure fluctuations with scleral depression may lead to corneal edema.
Clearing Vitreous Hemorrhage and Scleral Depression
Video credit: Sruthi Arepalli
- If a subhyaloidal hemorrhage is present, the hyaloid can be incised nasal to the disc or in an area of maximal elevation away from the fovea and the hemorrhage can be aspirated out of this space while working to release the hyaloid from the incisional plane.
- While working to release the vitreous, pay attention to the underlying retinal and vitreous details to see if there are areas of retinal breaks, rhegmatogenous detachment, or taut membranes and/or traction which may alter your surgical planning.
- If the hyaloid has not released and there is no mid-peripheral elevation to work in, create a plane between the vitreous and the retina (preferably working over an attached area or the disc), and extend that out into the periphery. Some of these techniques are further detailed below.
Posterior vitrectomy and membrane dissection
- After removing the bulk of the peripheral traction, the posterior vitreous can be trimmed down with the cutter.
- Some surgeons prefer to leave a tail of vitreous overlying the optic nerve to help induce a posterior vitreous detachment if necessary and/or appropriate given the amount of posterior traction. Caution should be used when removing the posterior hyaloid, as it is often very taut and has multiple adhesions, which can cause iatrogenic breaks if stripped too quickly. If there are multiple points of adhesions, it is often better to segment around the areas of fibrovascular proliferation.
Trimming Down Posterior Vitreous
Video credit: Sruthi Arepalli
- It is important to remove the posterior hyaloid, either through creating a posterior vitreous detachment or segmentation and delamination as this can act as a scaffold for recurrent traction and detachments.
- Membrane dissection can be approached from the “inside-out” or the “outside-in” method. Two main techniques to release retinal traction from membranes are segmentation (splitting the areas of traction/membranes into small islands) and delamination (removing these islands from the retina).
- Multiple instruments can be used to segment and delaminate fibrovascular proliferations and the posterior hyaloid, including a vitrector (smaller gauge with beveled tip can provide dissection of planes in conjunction with a high cut rate and low aspiration), horizontal or vertical scissors, forceps, a lighted pick, or viscodissection for flat, broad planes of adhesion.
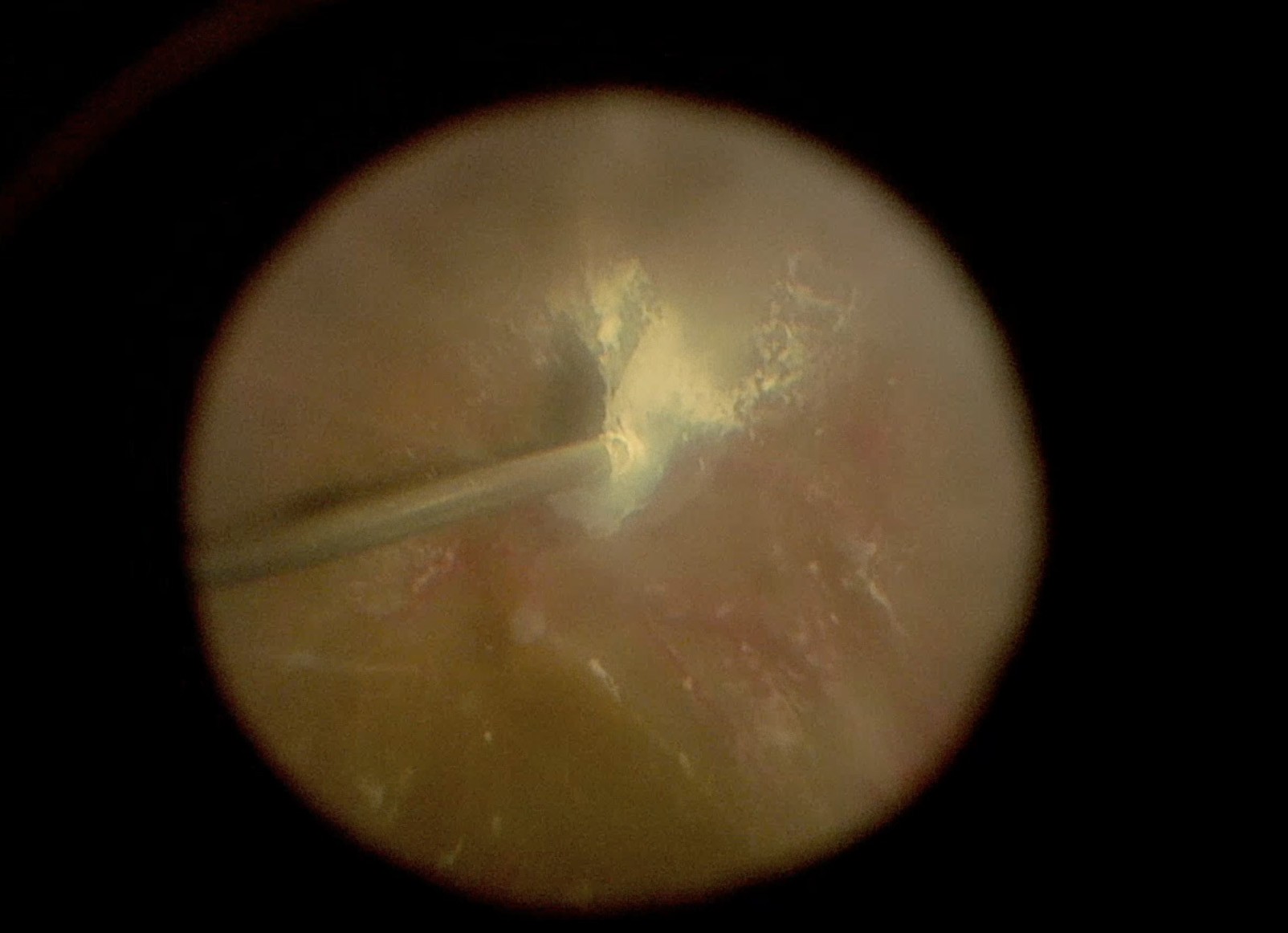
Figure 5: In this TRD a smaller gauge vitrectomy (27 G) is used which allows the tip of the cutter to be brought closer to the retina. This better assists in delineating fibrovascular proliferations off the retina. In this surgical photo the tip of the cutter is being used as a pic an scissors to segment down the fibrovascular tissue. Image Credit: Sruthi Arepalli
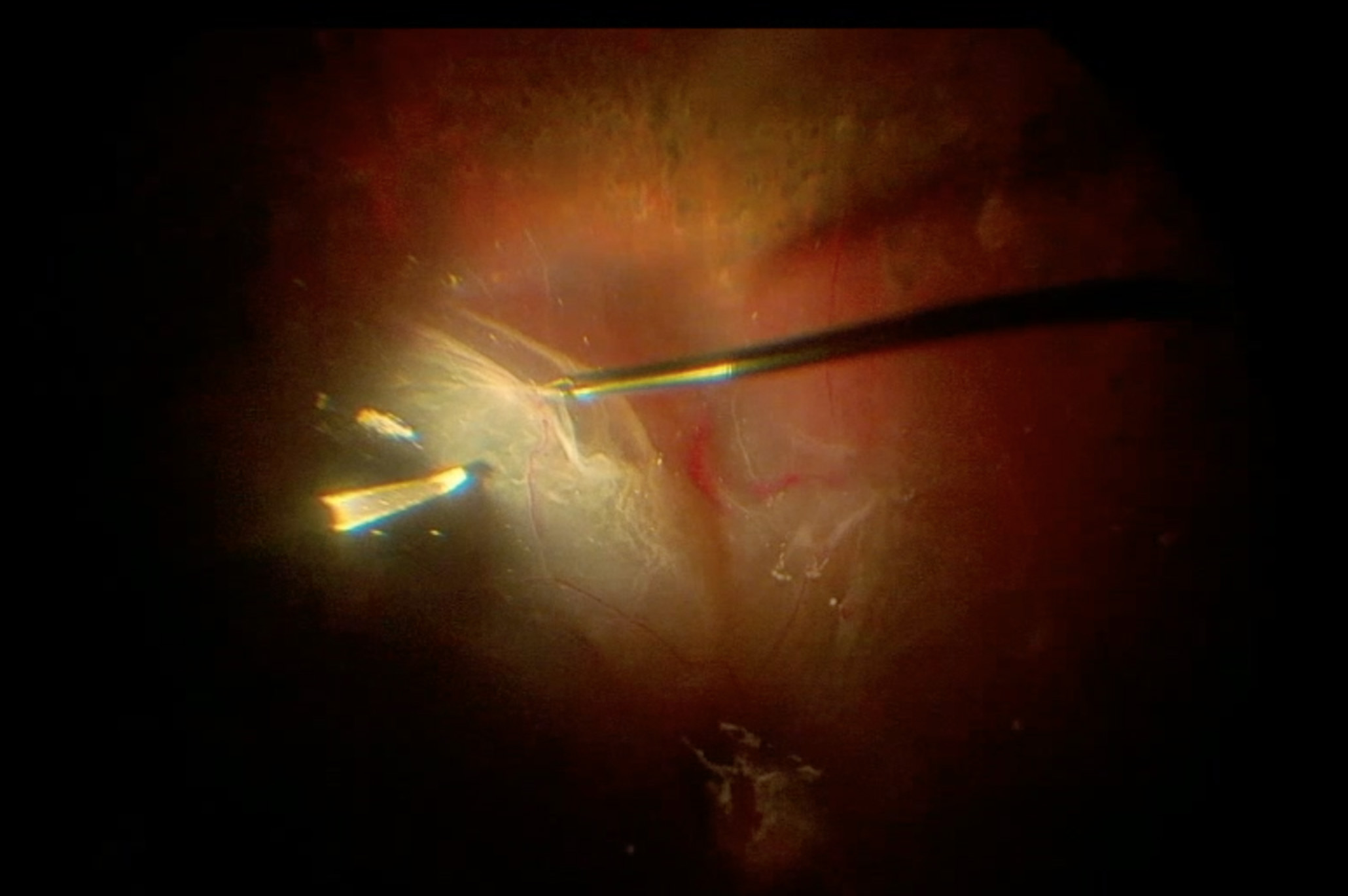
Figure 6: In this surgical photo during a TRD repair, the surgeon uses the bimanual technique with forceps and a pic to better remove tractional membranes from the retina. Image Credit: Thanos Papakostas
Segmentation
- To segment enter where there is enough space to place the instrument of choice between the fibrovascular membranes and the retina. Turn the cutter away from the retina and gently engage the membranes with the mouth of the cutter to start cutting. In areas of dense fibrosis, a decreased cut rate may be necessary. If using scissors, place one blade underneath the membrane (between the membrane the retina) and close the scissors on the fibrovascular proliferation. Continue to segment an island of tissue away from the retina.
Segmentation and Drainage in a TRD + RRD
Video credit: Thanos Papakostas; Editing and Narration: Sruthi Arepalli
TRD Segmentation and Delamination
Video credit: Thanos Papakostas
TRD Segmentation
Video credit: Andrew Zheng and Sruthi Arepalli
- In cases of a combined tractional and rhegmatogenous detachment, start membrane segmentation in an attached area. This allows for better coutertraction to develop planes to carry out over the area of detached retina. It is essential to remove all areas of traction around retinal breaks. If these are not removed, the vitreous can contract and lead to re-opening of these in the post-operative period.
Segmentation and Drainage in a TRD + RRD
Video credit: Thanos Papakostas; Editing and Narration: Sruthi Arepalli
TRD + RRD
Video credit: Thanos Papakostas; Editing and Narration: Sruthi Arepalli
Perfluorocarbon liquid (PFCL) can be used to help stabilize the retina in these cases as well, but the traction present in tractional retinal detachments increases the chances of subretinal accumulation of PFCL. If cases where peripheral dense membranes are unable to be removed given the number of retinal tears or thin retina, consider a retinectomy or scleral buckle to support these areas.
Delamination
- Delamination, or the removal of fibrovascular proliferation can be done through multiple techniques. The “fold-back” method involves placing the cutter on top of the island of tissue and allowing the free edges to enter the mouth of the cutter. The surgeon can also reflect and cut the membranes with scissors or a vitrector. Alternatively, they can peel the tissue with forceps if the adhesions are weak, or employ a bimanual method with forceps and scissors to reflect and cut areas of adhesions. The fold-back method is often very safe. If using scissors, do not spread the blades excessively under the membranes as these can cause trauma and breaks to the retina.
Segmentation and Drainage in a TRD + RRD
Video credit: Thanos Papakostas; Editing and Narration: Sruthi Arepalli
TRD Segmentation and Delamination
Video credit: Thanos Papakostas
- Not all areas need to be delaminated, however, if there are adjacent retinal tears it is prudent to remove the fibrovascular proliferations to reduce traction on that area.
ILM peel
- In certain cases, removing the ILM can further remove the scaffold for recurrent neovascularization and traction. It is also useful in cases of macular hole associated detachments. This is not always necessary and the benefits should be weighed against the risks.
Hemostasis
- If bleeding obscures the view, gently apply cautery to areas of bleeding vessels. Cautery can also be used to mark retinal tears.
- Intraoperative hemostasis can also be obtained by increasing the infusion pressure, but attention should be paid to the disc perfusion and used cautiously, especially in those with a history of glaucoma. Increased intraocular pressure can also cause corneal edema.
- Gentle aspiration or reflex can be used remove or displace hemorrhage as well especially once clotted.
- An air-fluid exchange can also help remove intraocular hemorrhage and wide the view for endolaser application.
Endolaser
- Apply laser around areas of retina tears after removing all traction from these areas.
Segmentation and Drainage in a TRD + RRD
Video credit: Thanos Papakostas; Editing and Narration: Sruthi Arepalli
TRD + RRD
Video credit: Thanos Papakostas; Editing and Narration: Sruthi Arepalli
- Apply panretinal photocoagulation to untreated areas, especially anteriorly in those eyes with recurrent hemorrhage with scleral depression.
Endolaser
Video credit: Sruthi Arepalli
Tamponade
- Eyes may be left with air in cases without breaks. The air improves the peripheral view and provides a tamponade that can help prevent shake out hemorrhage.
- Gas or oil may be required in cases of multiple breaks or concurrent retinal detachment.
Anti-VEGF
- Some surgeons prefer to administer anti-VEGF at the end of the case to prevent post-operative hemorrhage and treat any areas of active neovascularization.
- It is important to remember that a vitrectomized eye allows for a faster dissipation of anti-VEGF.
- Some surgeons prefer to administer a lower dose (i.e., a half dose of anti-VEGF) in eyes with a tamponade, as they believe the medication will be concentrated within the air-fluid interface.
Wound closure
- Wound closure is preferred to prevent post-operative hypotony, which can increase bleeding risk.