IMAGE OF THE MONTH: August 2022
A woman with no visual complaints


A 53 year old woman was referred for retinal eval. She had no visual complaints. On exam, visual acuity was 20/20 OU and anterior segment exam was within normal limits.
DIAGNOSIS
Optic Disc Pit with Associated Schisis Maculopathy
Discussion
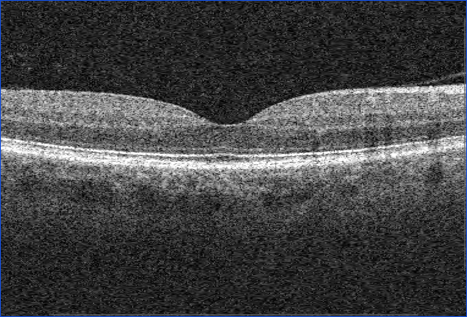
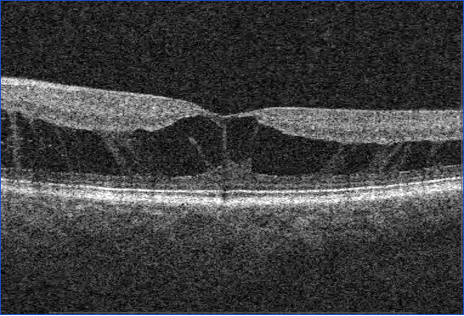
This patient had an optic disc pit in temporal aspect of nerve with associated schisis maculopathy. There was no associated retinal subretinal fluid. Given she was asymptomatic and stable over the course of her visits, the decision was made to observe closely.
Optic nerve pits are rare congenital defects thought to arise from a defect in embryogenesis, possibly an incomplete closure of the embryonic fissure [1]. While no specific risk factors have been identified, there have been reports of families with multiple affected members [2, 3]. When isolated, optic nerve pits are frequently asymptomatic although they may be associated with central or arcuate scotoma, or an enlarged blind spot. However, they can be associated with fluid accumulation within and beneath the retina at the macula and decreased vision [3]. The pathophysiology of this fluid accumulation is unknown, though theories include leakage from the CSF, vitreous cavity, or nearby dural vessels resulting from vitreous traction or pressure gradients [1, 2]. Maculopathy tends to arise around 30-50 years of age and can be seen 25-75% of patients with optic nerve pits [2].
Optic pits are often discovered incidentally, and may be seen with direct or indirect ophthalmoscopy, though they are best visualized on slip lamp exam [1]. Exam demonstrates an oval or round grey depression in the nerve head, most commonly inferotemporally [2, 3]. Maculopathy is more common with temporally located pits and can be detected using optical coherence tomography (OCT) showing intraretinal and subretinal fluid [2]. Serial OCTs and Humphrey visual fields may help rule out alternative diagnoses such as acquired optic disc pit from glaucoma [1].
Treatment is indicated with persistent decline in vision. Vitrectomy with light peripapillary laser has been shown to be the most effective in resolution of fluid. The resolution of fluid oftentimes lags significantly after vitrectomy.
1. Optic Pits - EyeWiki. Accessed May 22, 2022. https://eyewiki.aao.org/Optic_Pits
2. Moisseiev E, Moisseiev J, Loewenstein A. Optic disc pit maculopathy: when and how to treat? A review of the pathogenesis and treatment options. International Journal of Retina and Vitreous. 2015;1(1):13. doi:10.1186/s40942-015-0013-8
3. Kalogeropoulos D, Ch'ng SW, Lee R, et al. Optic Disc Pit Maculopathy: A Review. The Asia-Pacific Journal of Ophthalmology. 2019;8(3):247-255. doi:10.22608/APO.2018473