IMAGE OF THE MONTH: May 2024
How would you manage this patient?


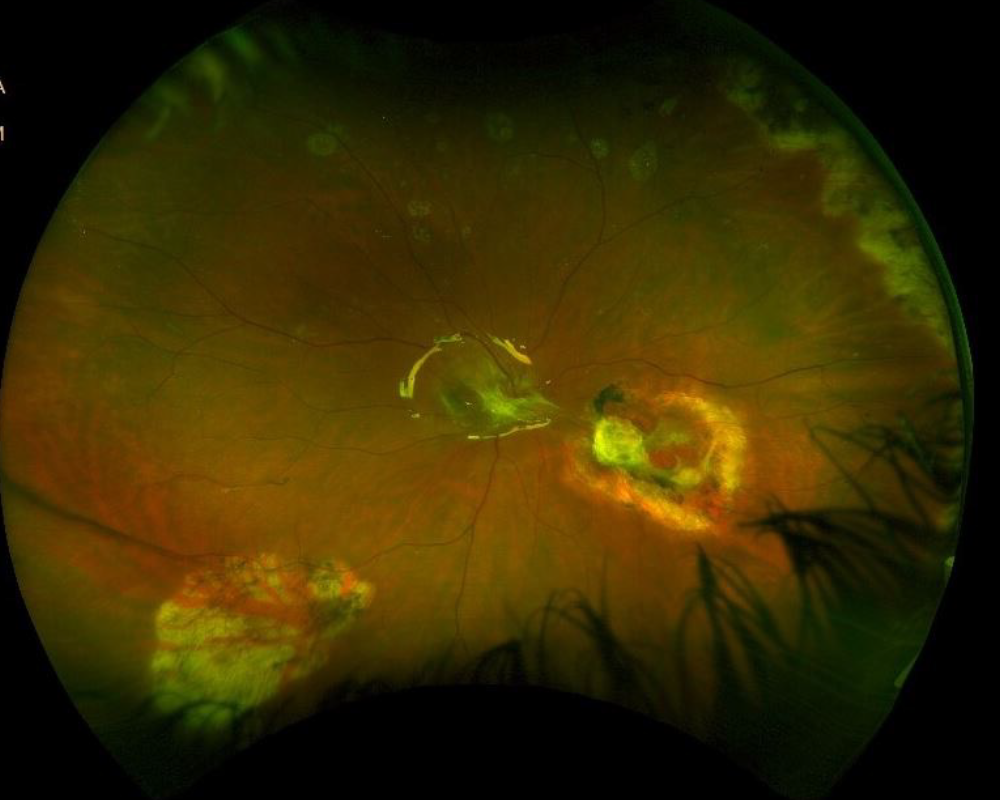
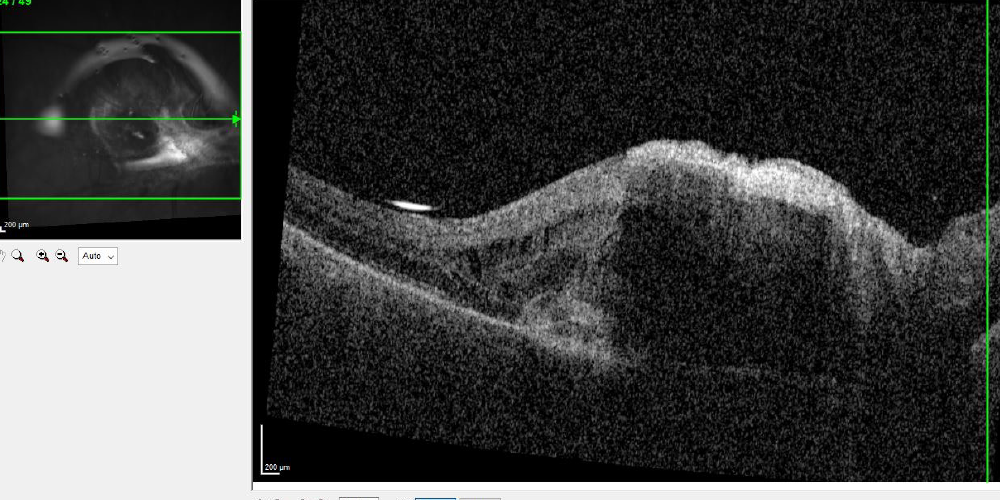
A 37-year-old female presents with a prior history of endogenous endophthalmitis (from staphylococcus pasteuri). She had initially undergone multiple intravitreal antibiotic injections and later a 25 g PPV/vitreous biopsy. Five months after vitrectomy she developed a rhegmatogenous retinal detachment, for which she underwent a vitrectomy, scleral buckle, lensectomy, silicone oil, and a subsequent vitrectomy, membrane peeling, relaxing retinotomy with oil for PVR. In the post operative period she developed a tractional band overlying the optic nerve that extended from the macula to the inferonasal retinotomy, which remained stable and was thus observed for over a year. She subsequently developed progressive macular subretinal fluid under a fibrotic tractional membrane with retinal thickening. What is the etiology and what would your management plan be?
DIAGNOSIS
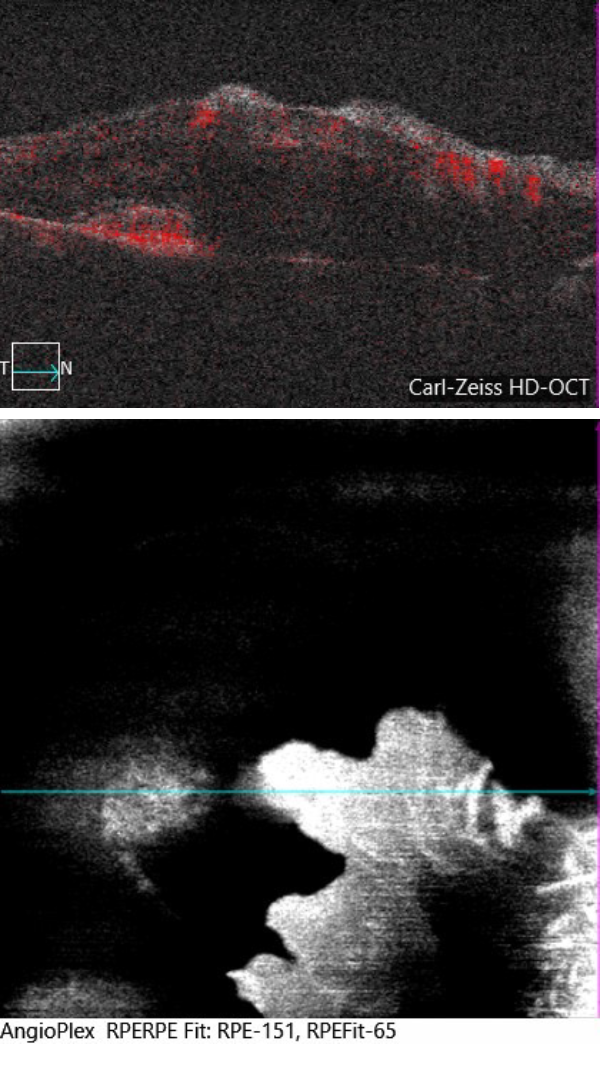
The patient underwent an OCT-A that showed flow within a vascularized PED as well as a nearby pocket of subretinal fluid and intraretinal fluid concerning for CNV formation. Due to concern for an active inflammatory choroidal neovascular membrane, she underwent a trial of anti-VEGF treatment. During her follow up visits, she was noted to have regression of the choroidal neovascular membrane and improvement in the intraretinal and subretinal fluid, confirming the diagnosis of a secondary inflammatory choroidal neovascular membrane.
CNV can occur in posterior segment inflammation, which is considered the third most common cause of CNV after age-related macular degeneration and myopia (1). OCT-A, in combination with fluorescein angiogram and OCT, can be helpful in identifying CNV lesions and differentiating them from inflammatory lesions (2). Anti-VEGF therapies should be considered in treating inflammatory CNVs to prevent severe central vision loss. Anti-VEGF treatment for inflammatory CNV is often used in combination with additional anti-inflammatory therapies (corticosteroids or immunosuppressive medication) (3).
1.Perentes Y, Van Tran T, Sickenberg M, Herbort CP. Subretinal neovascular membranes complicating uveitis: Frequency, treatments, and visual outcome. Ocul Immunol Inflamm. 2005;13:219–24
2.Astroz P, Miere A, Mrejen S, Sekfali R, Souied EH, Jung C, Nghiem-Buffet S, Cohen SY. OPTICAL COHERENCE TOMOGRAPHY ANGIOGRAPHY TO DISTINGUISH CHOROIDAL NEOVASCULARIZATION FROM MACULAR INFLAMMATORY LESIONS IN MULTIFOCAL CHOROIDITIS. Retina. 2018 Feb;38(2):299-309. doi: 10.1097/IAE.0000000000001617. PMID: 28368976.
3.Agarwal A, Invernizzi A, Singh RB, Foulsham W, Aggarwal K, Handa S, Agrawal R, Pavesio C, Gupta V. An update on inflammatory choroidal neovascularization: epidemiology, multimodal imaging, and management. J Ophthalmic Inflamm Infect. 2018 Sep 12;8(1):13. doi: 10.1186/s12348-018-0155-6. PMID: 30209691; PMCID: PMC6135736.