IMAGE OF THE MONTH: April 2025
What's the spot(s)?


Case
A 32-year-old male with unknown past medical is referred for evaluation of a “macular scar” in the left eye. Visual acuity is 20/20 OU and the patient does not have any visual complaints. What is the diagnosis? And what systemic work-up would you consider?
Diagnosis
Torpedo maculopathy and pisiform congenital hypertrophy of the retinal pigment epithelium (CHRPE) in the setting of Gardner’s Syndrome
Discussion
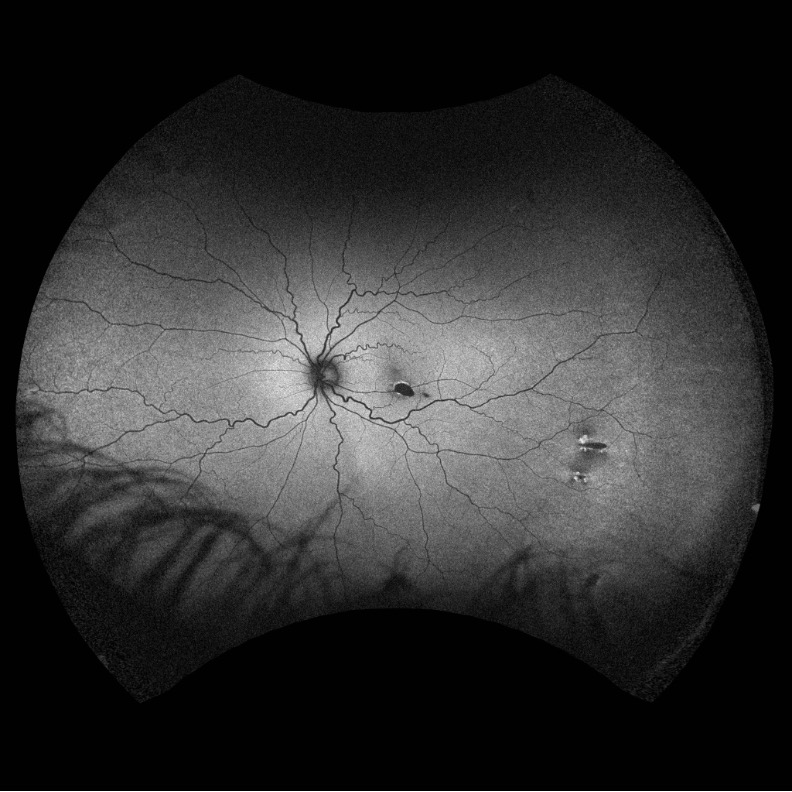
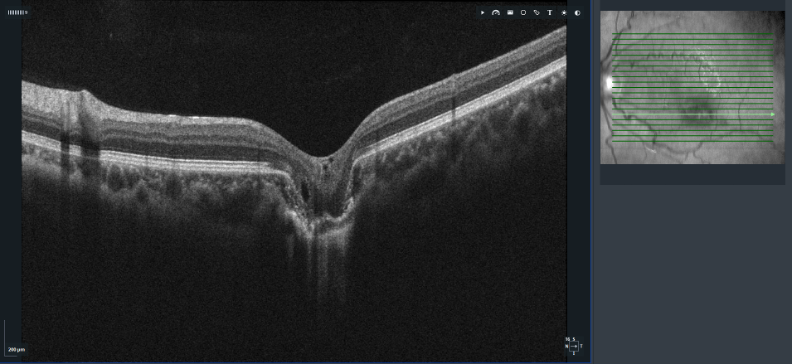
The differential diagnosis for pigmented retinal lesions includes RPE hamartoma, choroidal nevus, choroidal melanoma, focal pigmentation or chorioretinal scarring from prior inflammation or injury, torpedo maculopathy, and congenital hypertrophy of the RPE (CHRPE). Fundus autofluorescence revealed marked absolute hypofluorescence of the torpedo-shaped macular lesion, consistent with RPE absence (as opposed to just disruption as might be seen in a focal choroidal excavation), while the peripheral lesions demonstrate central absolute hypofluorescence surrounded by peripheral hyperautofluorescence along their halo-tail margins. OCT through the macular lesion shows outer retinal thinning, RPE absence, and focal choroidal tissue absence without subretinal fluid. Given these imaging features, and the presence of additional peripheral, pigmented fleck-like lesions in the fellow eye, two diagnoses were made: torpedo maculopathy and pisiform CHRPE.
Torpedo maculopathy is a congenital lesion typically located temporal to the fovea, characterized by a horizontally oval, torpedo-shaped appearance. These lesions have been subclassified into two main types: type 1 exhibits attenuation of the ellipsoid and interdigitation zones without cavitation, while type 2, as seen in this patient, demonstrates outer retinal cavitation due to choroidal tissue absence with loss of photoreceptor integrity and RPE.
The peripheral CHRPE lesions also exhibited classic features of concern—a pisiform shape, directional orientation toward the optic nerve, and a surrounding halo-tail configuration—consistent with the spectrum of findings associated with familial adenomatous polyposis (FAP) and its variant, Gardner Syndrome.
Although torpedo maculopathy is generally benign and non-progressive, rare cases have been associated with the development of secondary choroidal neovascularization (CNV).¹˒² While this patient had no clinical or imaging evidence of CNV, he was educated about potential symptoms and provided with an Amsler grid for home monitoring. Notably, recent literature has proposed a potential developmental association between torpedo maculopathy and FAP variants, suggesting a shared pathogenesis involving RPE development.³ Given the patient’s 20/20 vision and absence of active pathology, no ocular treatment was indicated with the patient scheduled to follow-up for interval exams.
On questioning the patient revealed a family history of polyps, and he had already undergone prior colonoscopy years previously finding numerous polyps. Thus, they already carried a known diagnosis of Gardner syndrome at the time of presentation. Routine follow-up with gastroenterology was recommended.
Imaging
Ultra-widefield Fundus Autofluorescence Image (OS):
OCT Raster of Torpedo Lesion (OS):
1. Banaee T, Doss M, Eller AW. Torpedo maculopathy complicated by choroidal neovascularization. Am J Ophthalmol Case Rep. 2020 Jun 6;19:100772. doi: 10.1016/j.ajoc.2020.100772. PMID: 32551405; PMCID: PMC7287237.
2. Jurjevic D, Böni C, Barthelmes D, Fasler K, Becker M, Michels S, Stemmle J, Herbort C, Zweifel SA. Torpedo Maculopathy Associated with Choroidal Neovascularization. Klin Monbl Augenheilkd. 2017 Apr;234(4):508-514. English. doi: 10.1055/s-0043-100230. Epub 2017 May 3. PMID: 28470647.
3. Packo K, Goldberg MF. Torpedo-like lesions in the ocular fundi of Gardner syndrome: hiding in plain view. Ophthalmic Genet. 2021 Oct;42(5):514-520. doi: 10.1080/13816810.2021.1925930. Epub 2021 May 20. PMID: 34014136.