IMAGE OF THE MONTH: July 2022
Bilateral Color vision disturbance
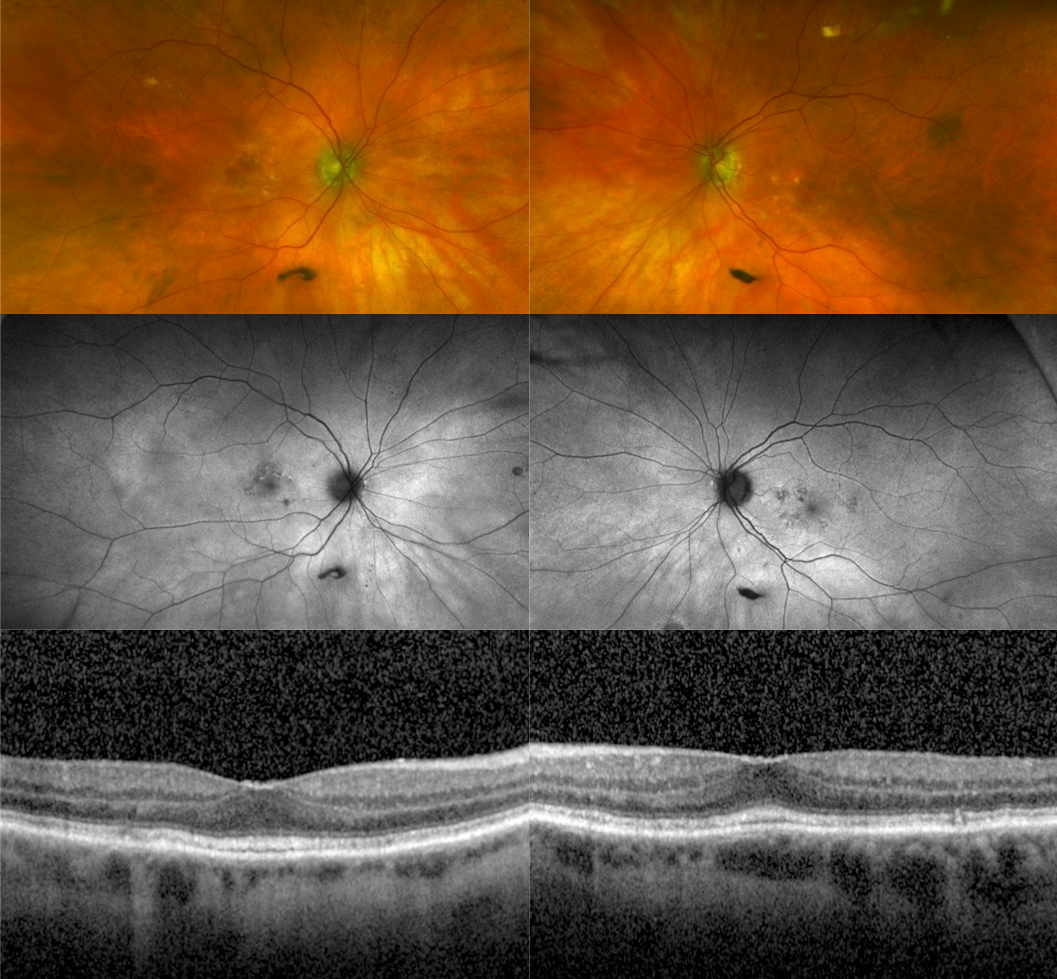
An 87-year-old female patient with past medical history notable for aortic stenosis, atrial fibrillation and nonexudative age-related macular degeneration attends for routine scheduled follow-up and describes three-weeks of color vision disturbance, as well as generally blurry vision in both eyes. Best-corrected visual acuity was found to be 20/40 in both eyes, down from her baseline of 20/25. Color plates were noted to be 2/10 and 1/10 in the right and left eyes, respectively. The fundus, autofluorescence and OCT images are shown below. What is the diagnosis?
DIAGNOSIS
Digoxin toxicity
Discussion
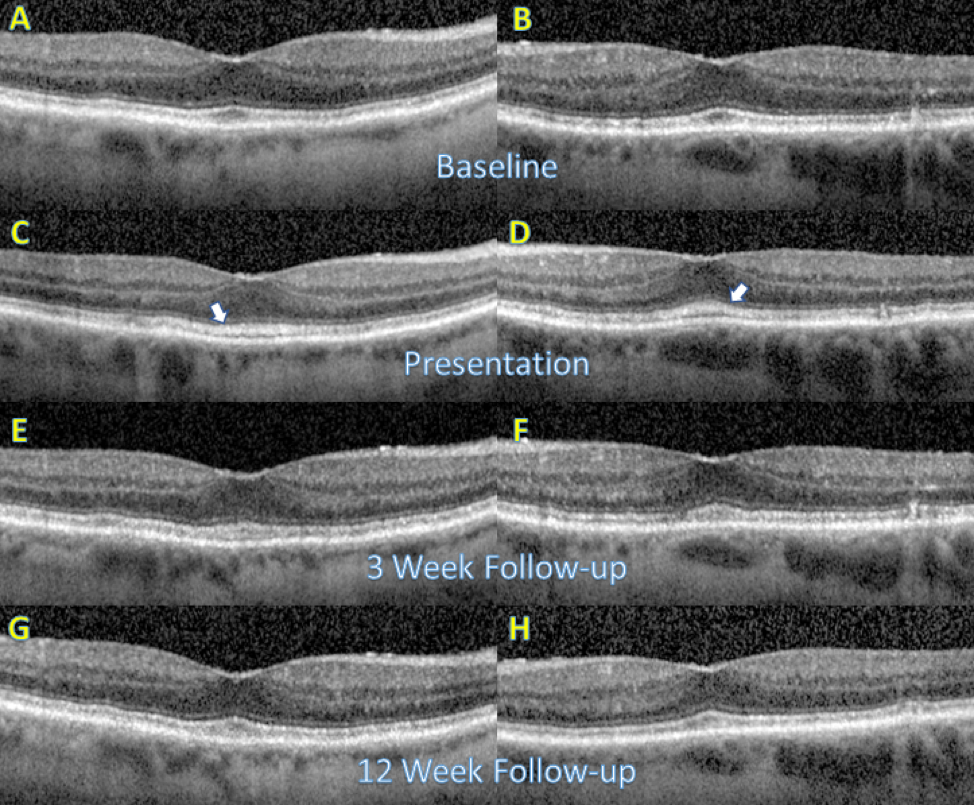
The imaging shown above is notable for a few drusen and pigmentary changes in the macula of both eyes, which was stable from OCT scans obtained at prior visits. Similarly, no change from the patient’s baseline was found on fundus autofluorescence. However, the OCT demonstrated new sub-foveal thickening and blurring of the ellipsoid zone in both eyes, with an accumulation of hyperreflective material in the photoreceptor outer segments (see figure below to compare her presentation to baseline OCT, obtained nine months prior). There was also some loss of definition of the interdigitation zone noted.
On further history taking, the patient relayed that one month prior to the onset of her visual symptoms the dose of her digoxin had been doubled to 250 micrograms daily, and amiodarone 300 milligrams twice daily had been introduced to her medical regimen in the setting of insufficiently controlled atrial fibrillation. Of note, amiodarone is a potentiator of digoxin. Based on the patient’s clinical history, the acute decrease in afferent visual function, as well as the imaging findings, a diagnosis of presumed digoxin toxicity was made and communicated to her cardiologist, who immediately stopped both the digoxin and amiodarone. Three weeks later, there was early normalization of initial findings on OCT, though her visual acuity did not show any improvement. At twelve-week follow-up, visual acuity had returned to her 20/25 baseline, color plates were full in both eyes, and the acute OCT changes had completely resolved.
Given the decreasing use of digoxin due to its narrow therapeutic window and the risk of toxicity, it is relatively rare to capture the structural OCT changes shown in this case. However, it is vital to be alert to the possibility of digoxin toxicity not only because of the risk of permanent visual effects, but because digoxin toxicity is potentially life-threatening.