CASE OF THE MONTH: October 2023
A Flying Saucer Sighting

Case Presentation
53 year-old woman presents with no vision complaints
History
- PMHx: rheumatoid arthritis, discoid lupus, nephrolithiasis
- POHx: none
- SHx: current smoker
- FHx: no known eye disease
- Allergies: None
- Rx: Plaquenil (hydroxychloroquine) use since 2001 (weight-based dosing = 4.47 mg/kg/day), fluticasone nasal spray
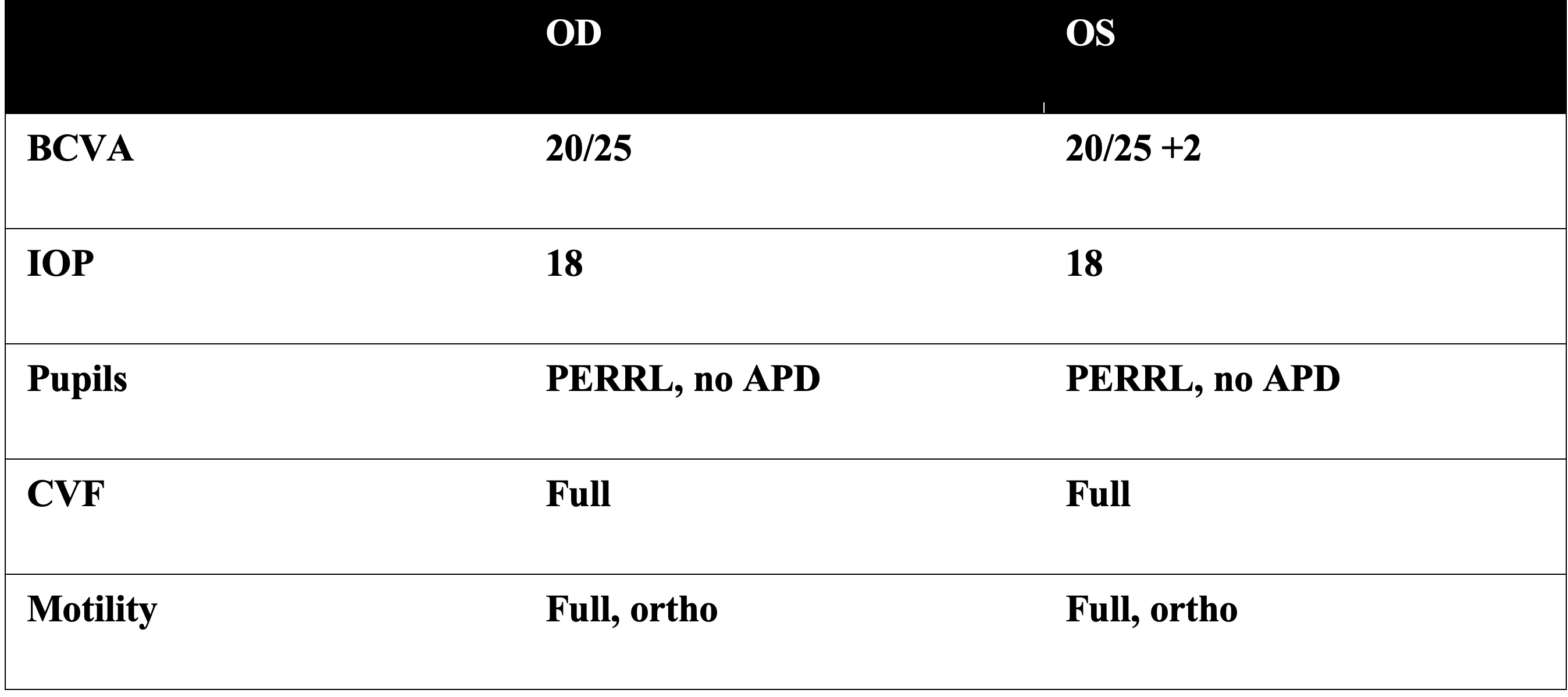
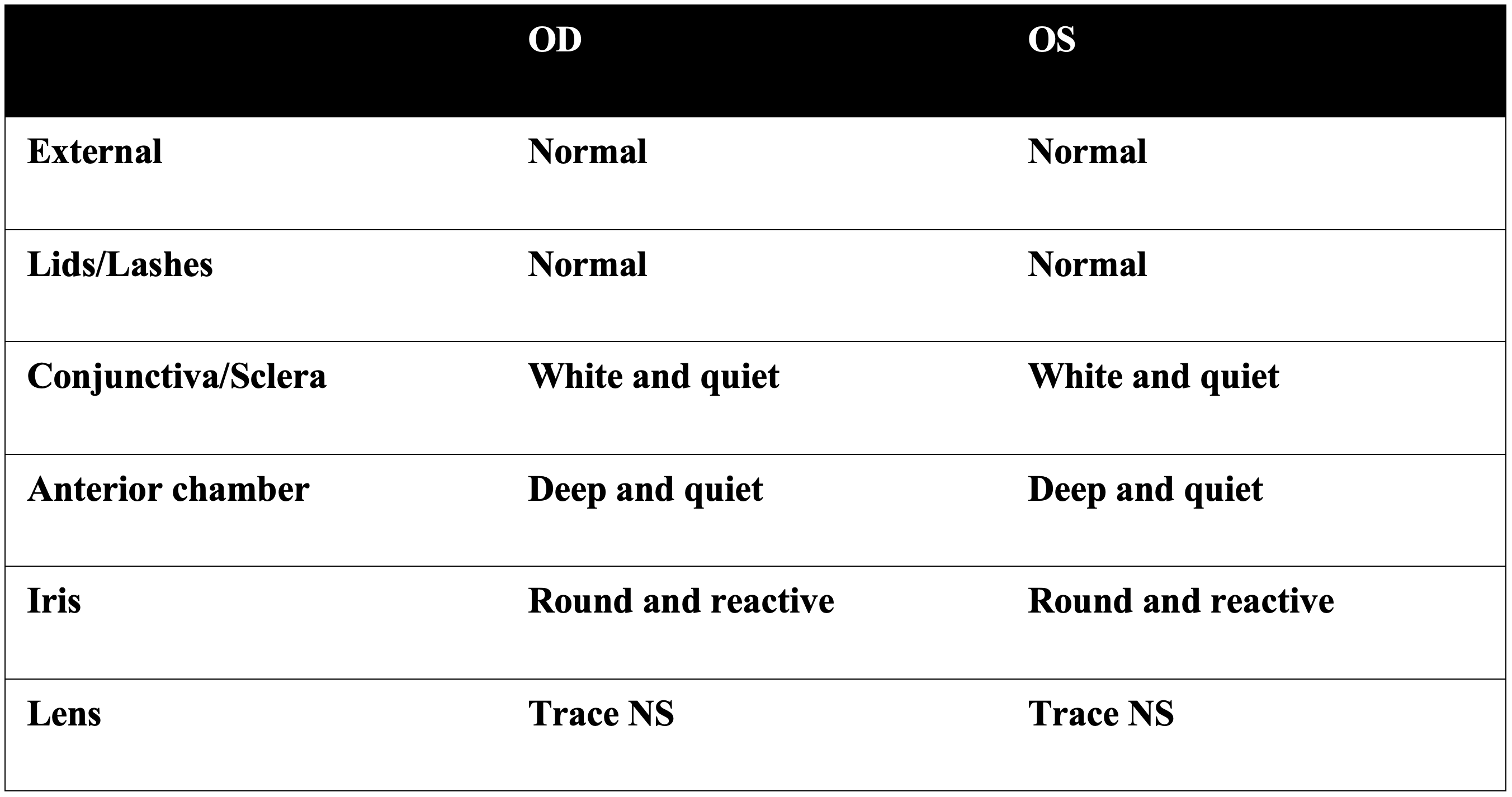
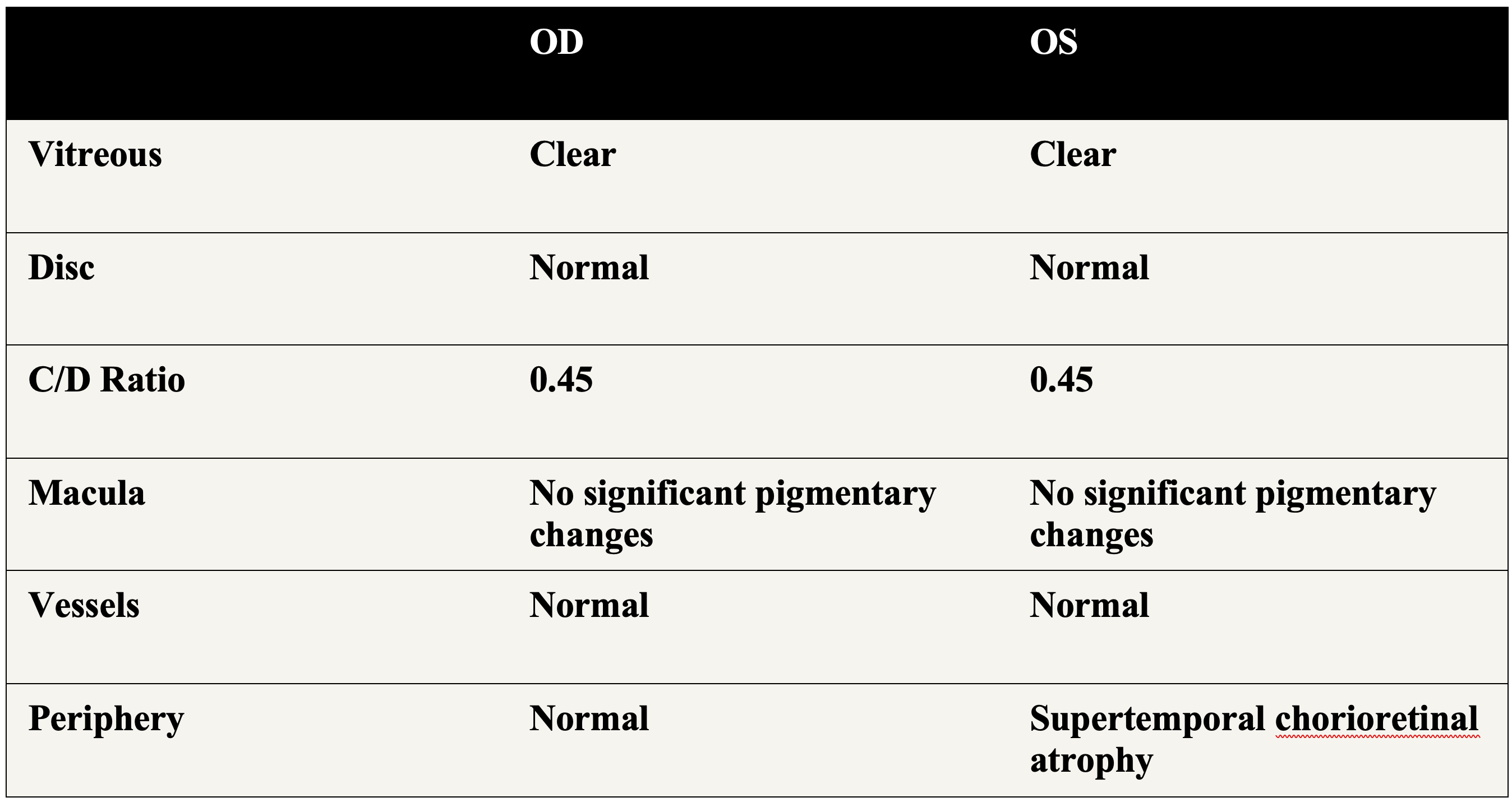
Exam
Summary of Findings
- 53-year-old woman presents for regular eye exam screening without vision complaints.
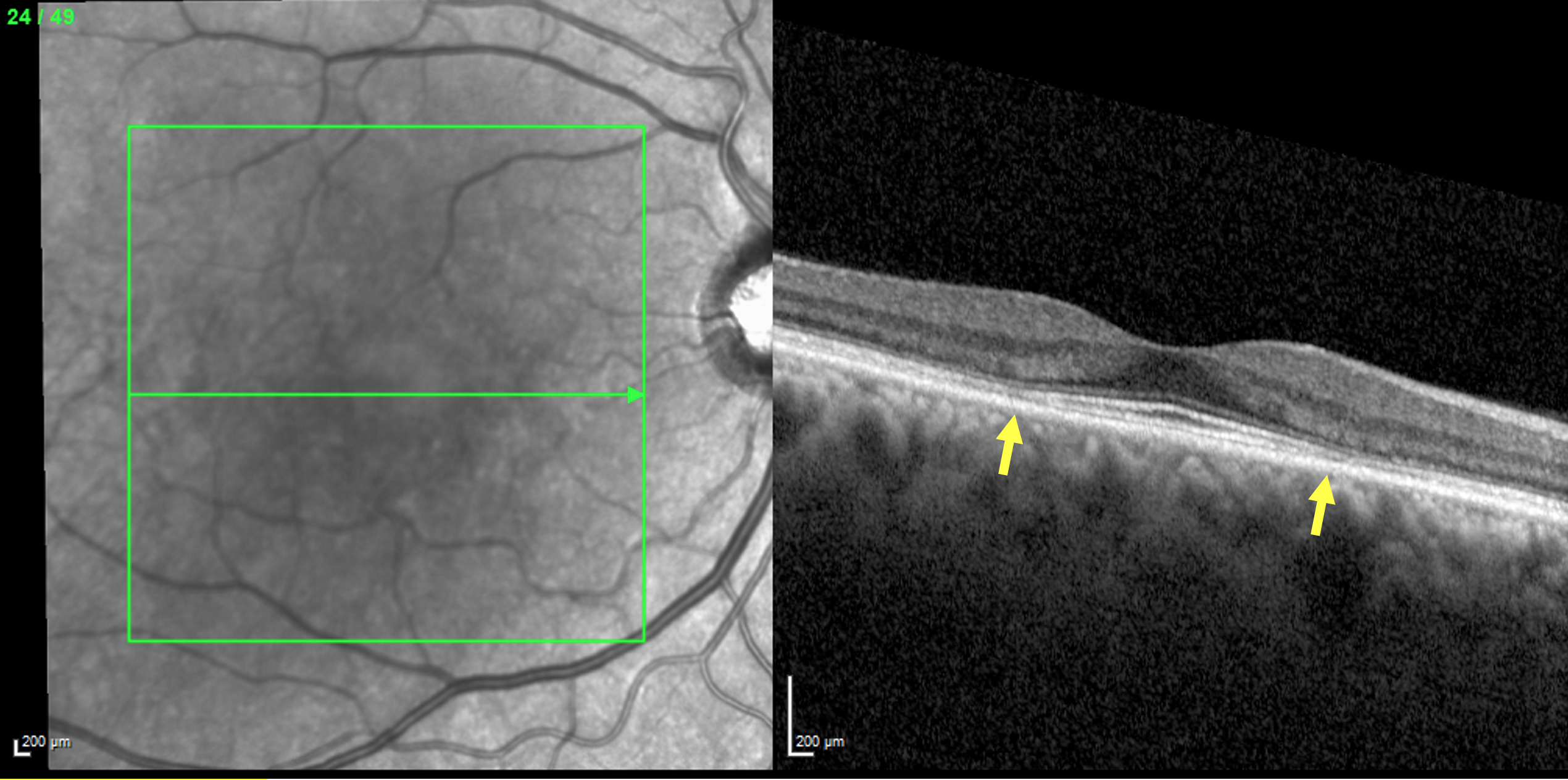
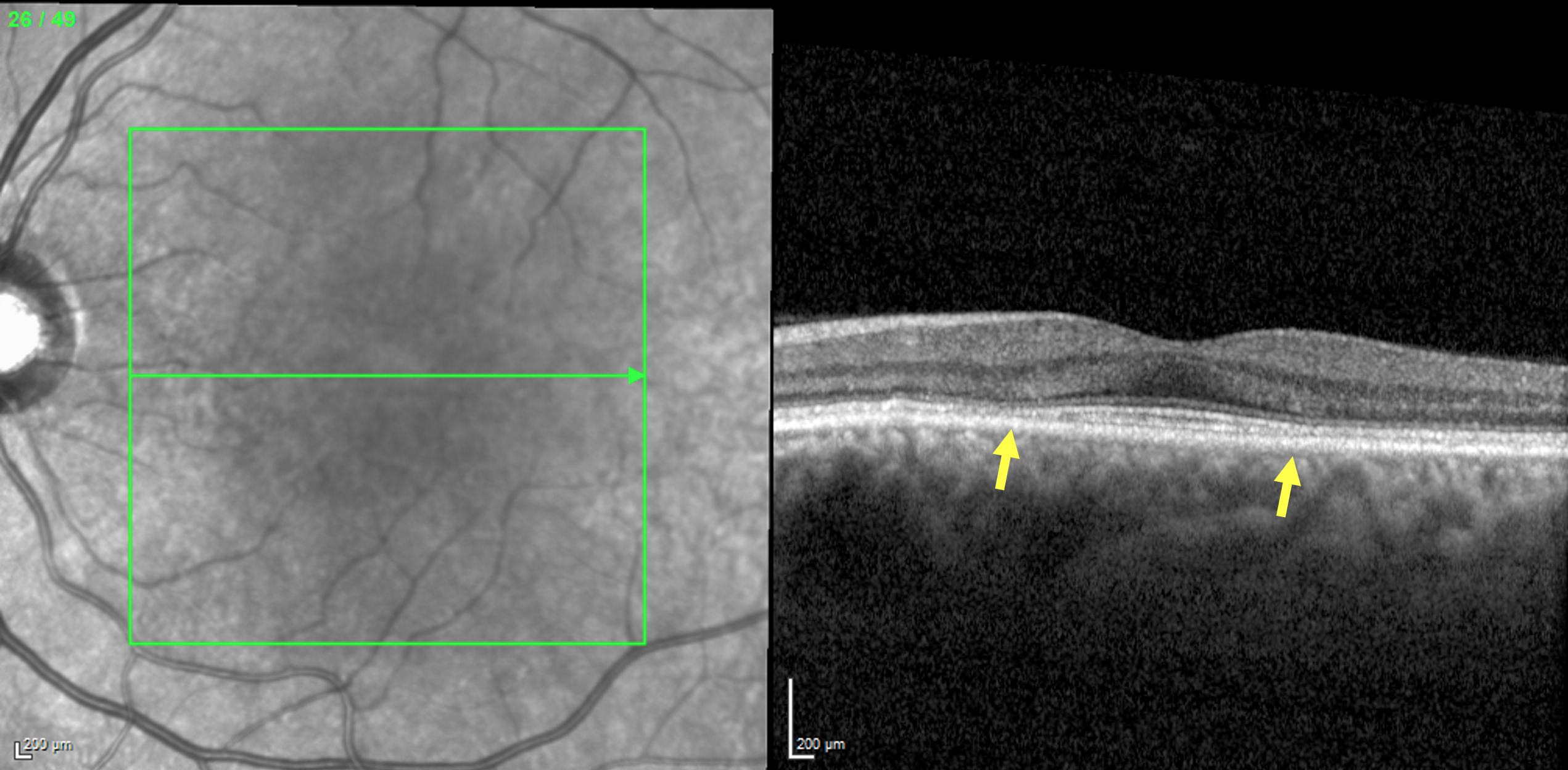
- OCT: Subtle perifoveal loss of ellipsoid zone with outer retinal thinning (yellow arrows) in both eyes
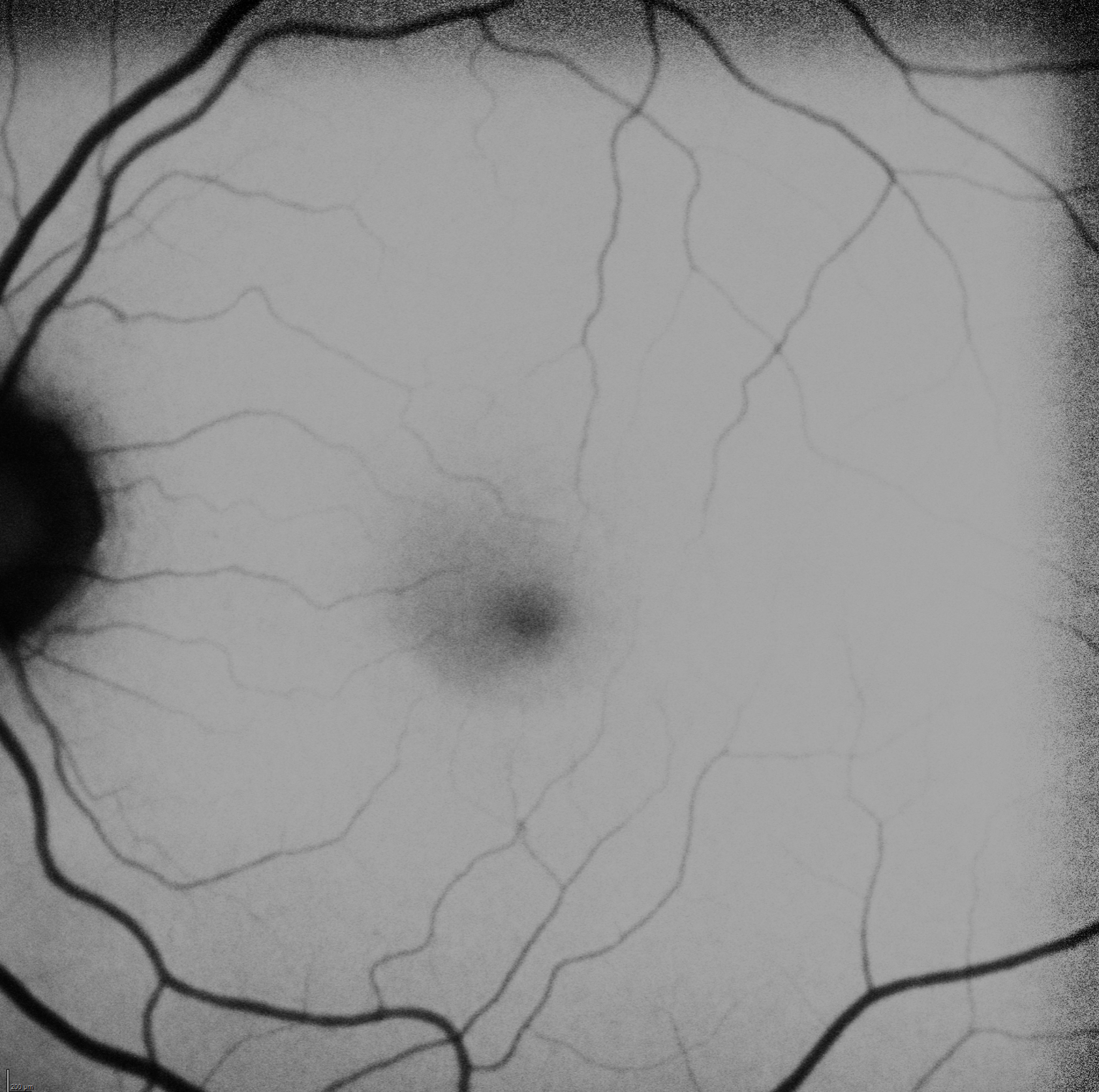
- Fundus autofluorescence: no frank abnormal hypo or hyper autofluorescence
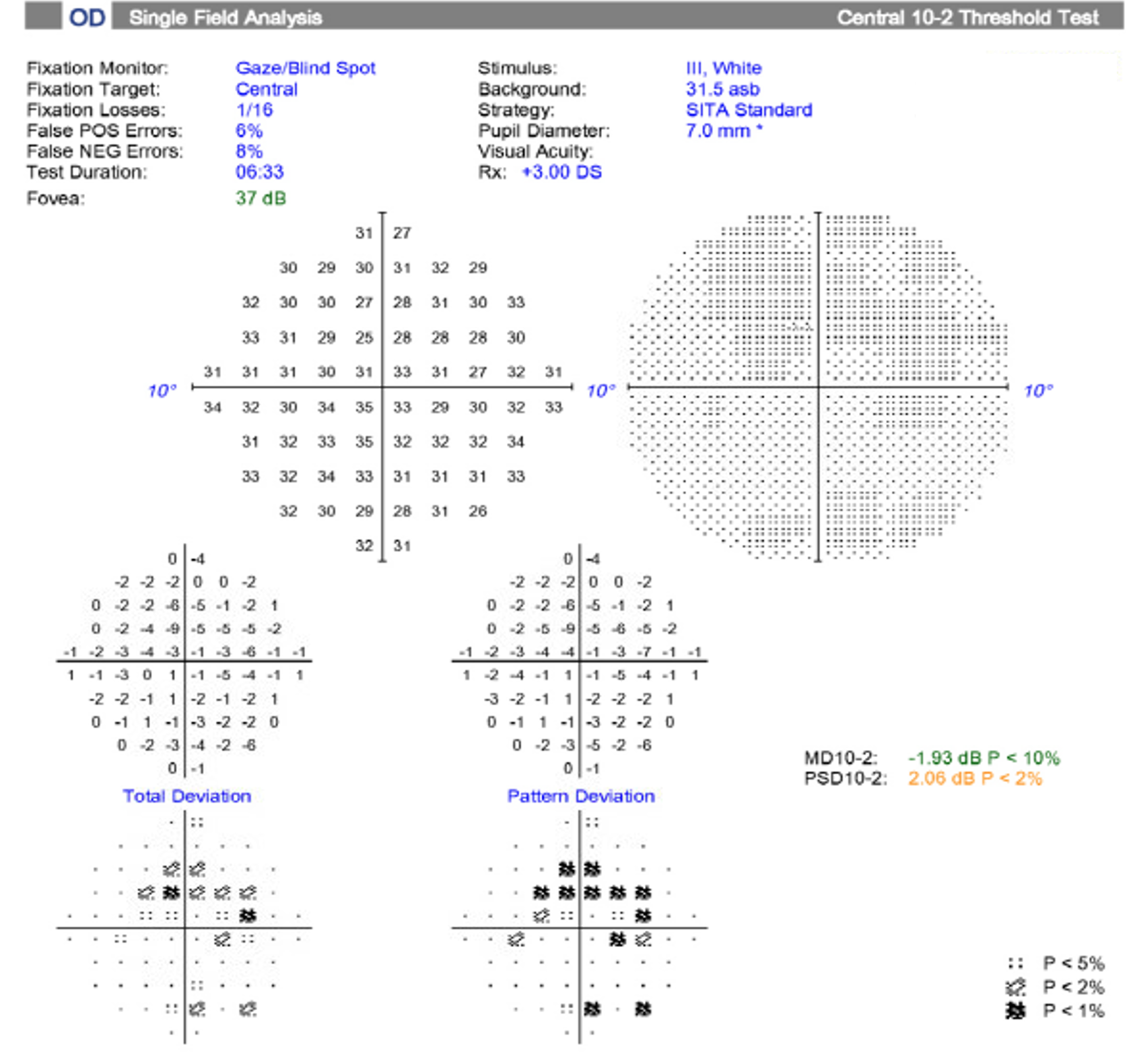
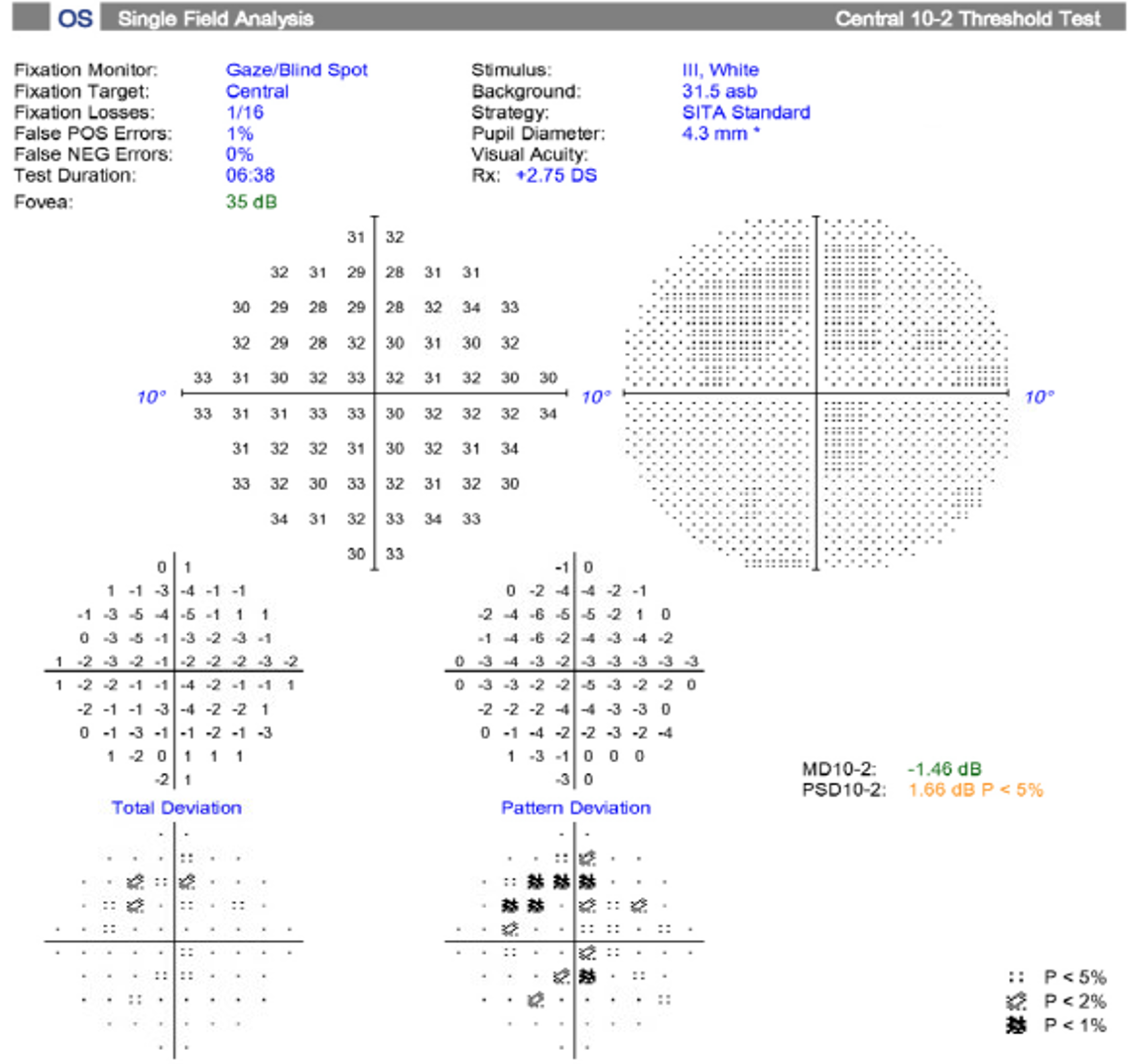
- HVF 10-2: Largely reliable testing in both eyes. Central depressions revealed in both eyes.
Mechanism and differential diagnosis
- Toxic maculopathy
- Hydroxychloroquine toxicity
- Chloroquine toxicity
- Degenerative
- Age-related macular degeneration
- Stargardt disease
- Cone dystrophy
- Central areolar choroidal dystrophy
Treatment & clinical course
- Clinical appearance concerning for Plaquenil (hydroxychloroquine) toxicity. Patient was advised to stop Plaquenil immediately. These findings were shared with the rheumatologist to find alternate treatment therapies.
- Diagnosis: Plaquenil (hydroxychloroquine) retinal toxicity
Discussion
- Hydroxychloroquine (Plaquenil) is a commonly prescribed medication for the treatment of inflammatory conditions.
- Retinal toxicity was first described in the late 1960s for Plaquenil1. As a result, regular screening for patients while taking the medicine is recommended. Unfortunately, once toxicity develops, it is irreversible; furthermore, it can continue to progress despite cessation of the medication. Early toxicity detection is paramount to try and limit the extent of vision loss.
- Risk factors
- The risk of development of toxicity is most influenced by daily weight-based dosing and duration of usage.
- Risk of toxicity decreases with dosages < 5mg/kg/day
- There is a lower risk of toxicity in the first 5 years of usage. The risk of toxicity up to 5 years is < 1%. It rises to < 2% up to 10 years but increases significantly to 20% at 20 years.2
- Other factors that increase the risk of toxicity include renal disease, concomitant tamoxifen usage, and preexisting macular disease.
- Screening recommendations: 2
- Baseline screening within 1st year of usage with full dilated exam, visual field and OCT
- Annual screening following 5 years of usage but sooner with any risk factors. Diagnostic imaging includes OCT, HVF 10-2, and autofluorescence. Consider HVF 30-2 testing for Asian patients due to increased prevalence of pathology extending outside of the central macula.3 Multifocal ERG can be employed as needed.
1. Shearer RV, Dubois EL. Ocular changes induced by long-term hydroxychloroquine (plaquenil) therapy. Am J Ophthalmol. 1967 Aug;64(2):245-52.
2. Marmor MF, Kellner U, Lai TY, Melles RB, Mieler WF; American Academy of Ophthalmology. Recommendations on Screening for Chloroquine and Hydroxychloroquine Retinopathy (2016 Revision). Ophthalmology. 2016 Jun;123(6):1386-94.
3. Melles RB, Marmor MF. Pericentral retinopathy and racial differences in hydroxychloroquine toxicity. Ophthalmology. 2015 Jan;122(1):110-6.