CASE OF THE MONTH: January 2024
Breakthrough Lesions

Chief Complaint
- Left eye blurry vision x 6 weeks
History of Present Illness
- 42M, saw outside ophthalmologist 6 weeks ago
- Diagnosed with uveitis OS
- Started on steroids and cycloplegic
- No improvement
- 11/10: Saw retina for second opinion
- Blurry vision OS>OD, floaters OS
- Left eye mild injection
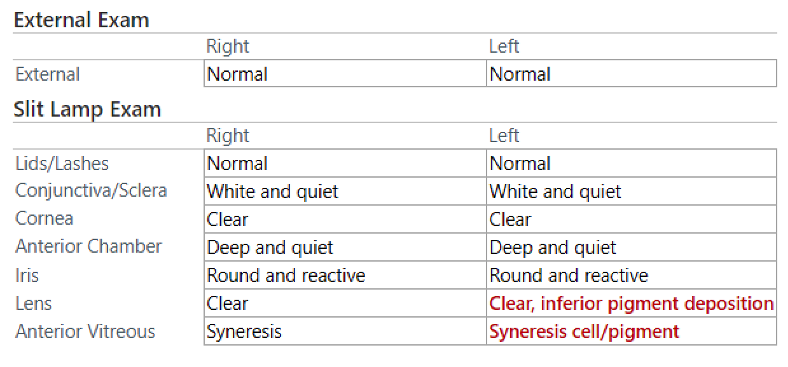
Exam
- VA (cc) 20/20-3, 20/40-1 ph 20/20
- IOP 12/9
- PERRL
- CVF full OU
- EOMI
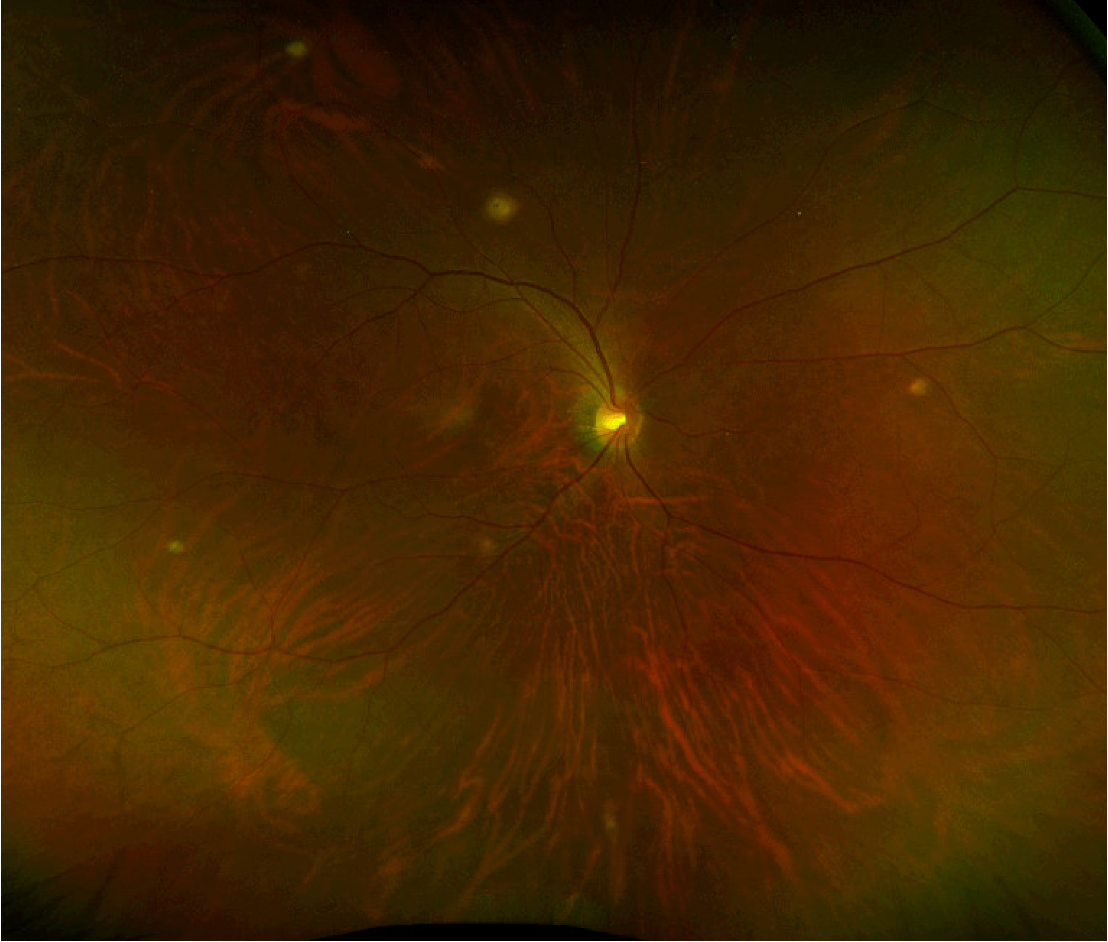
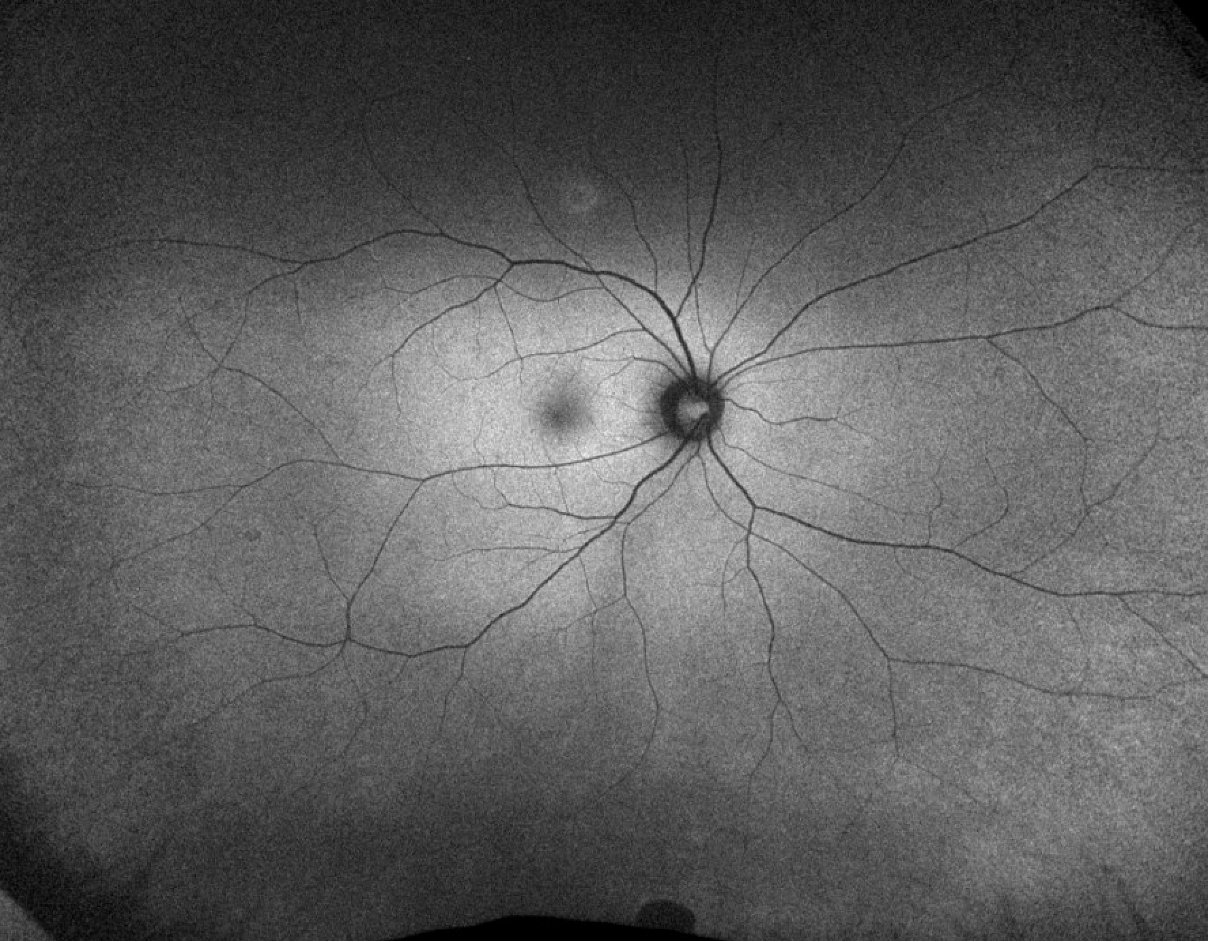
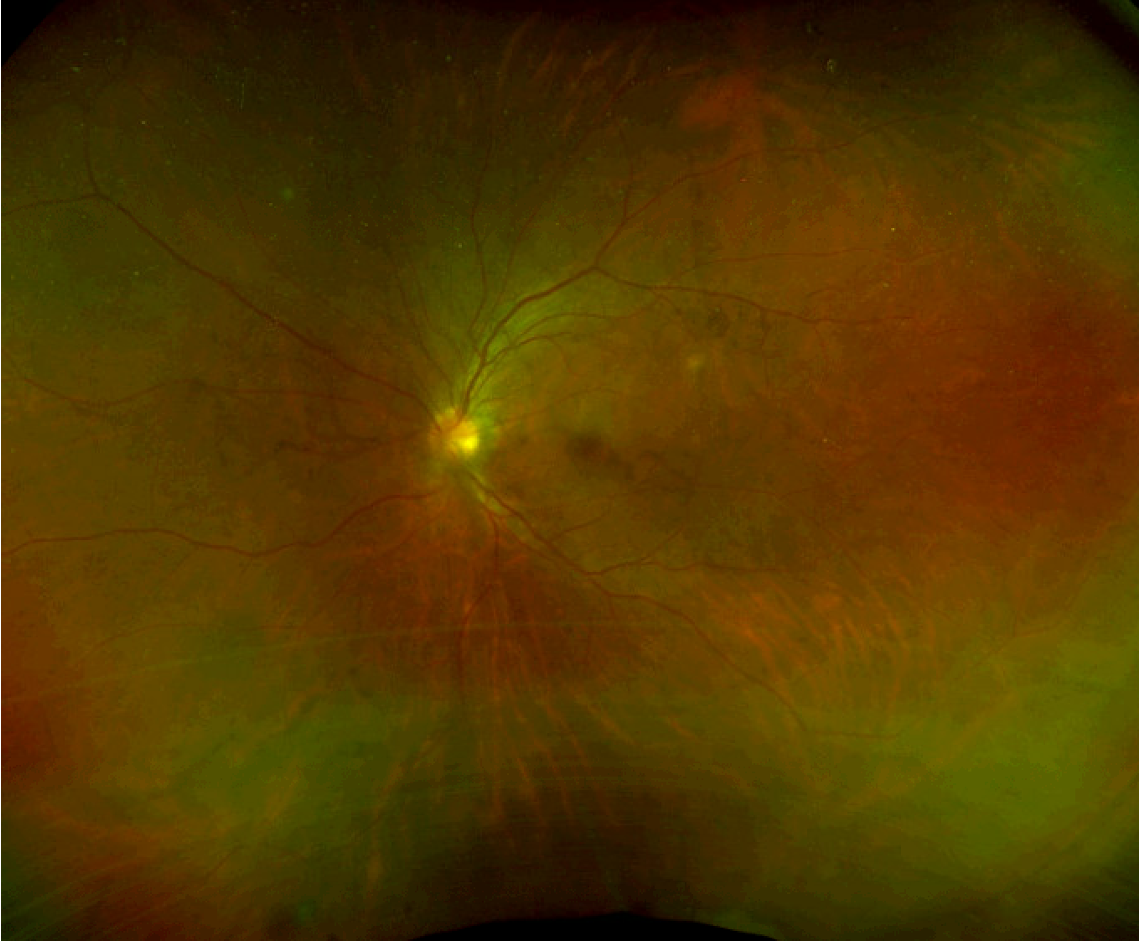
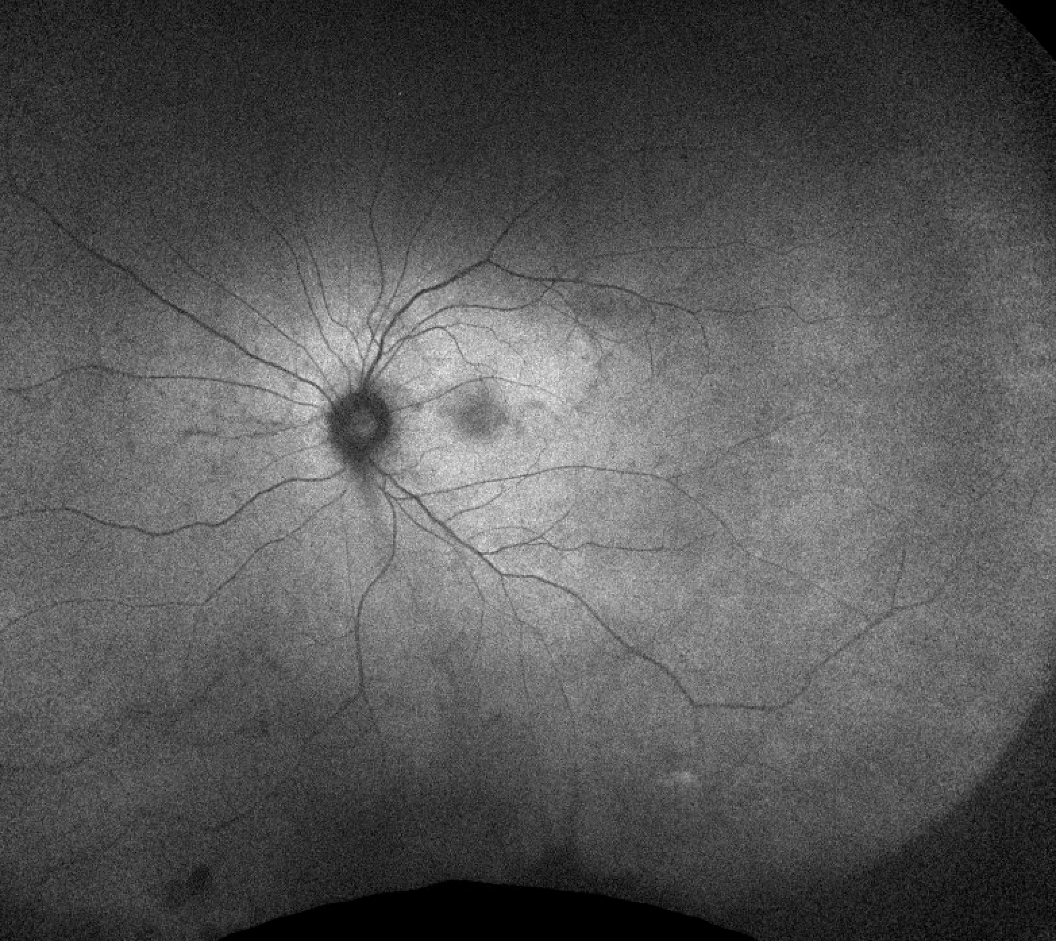
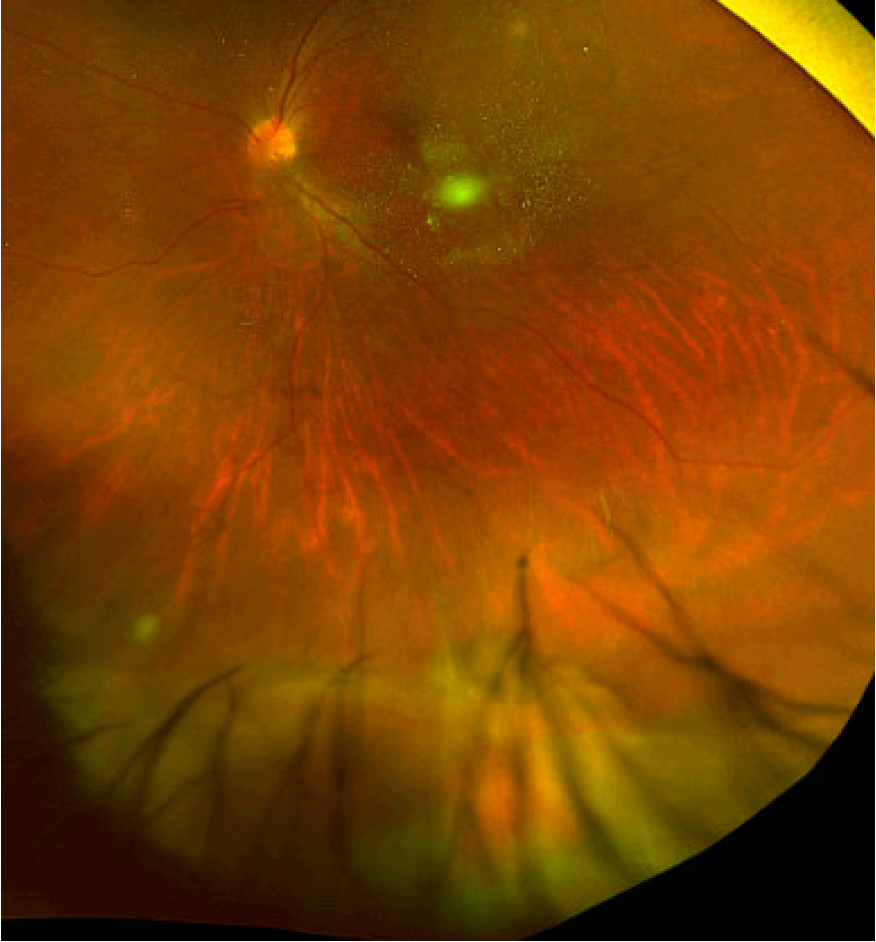
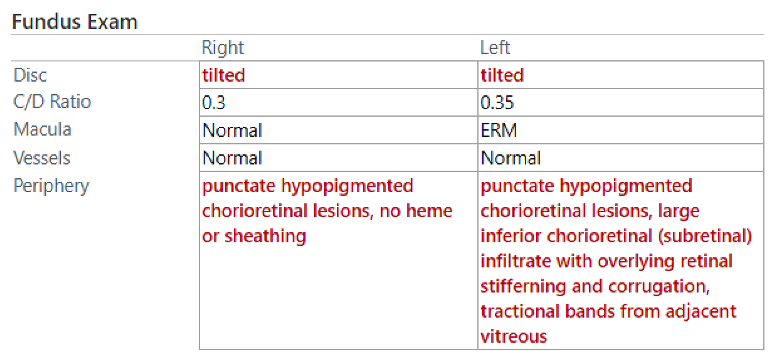
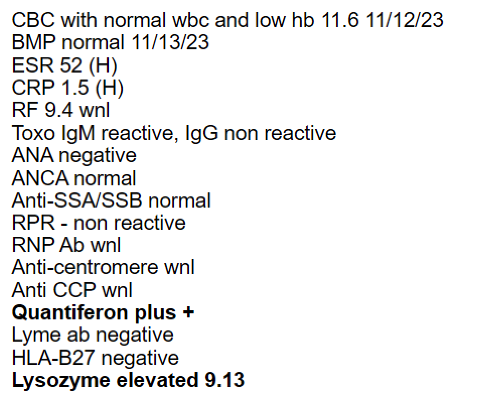
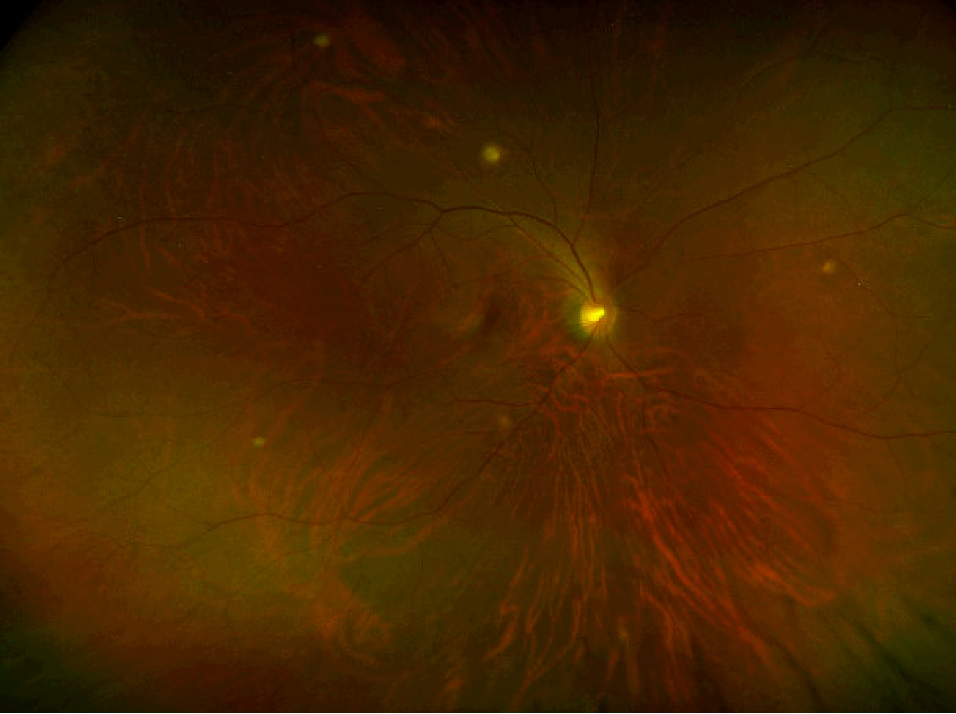
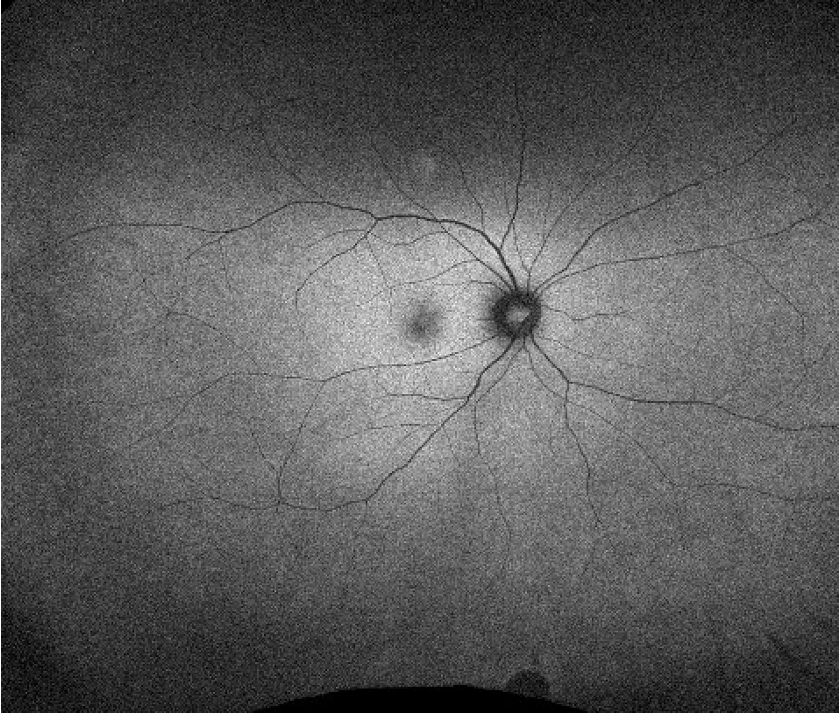
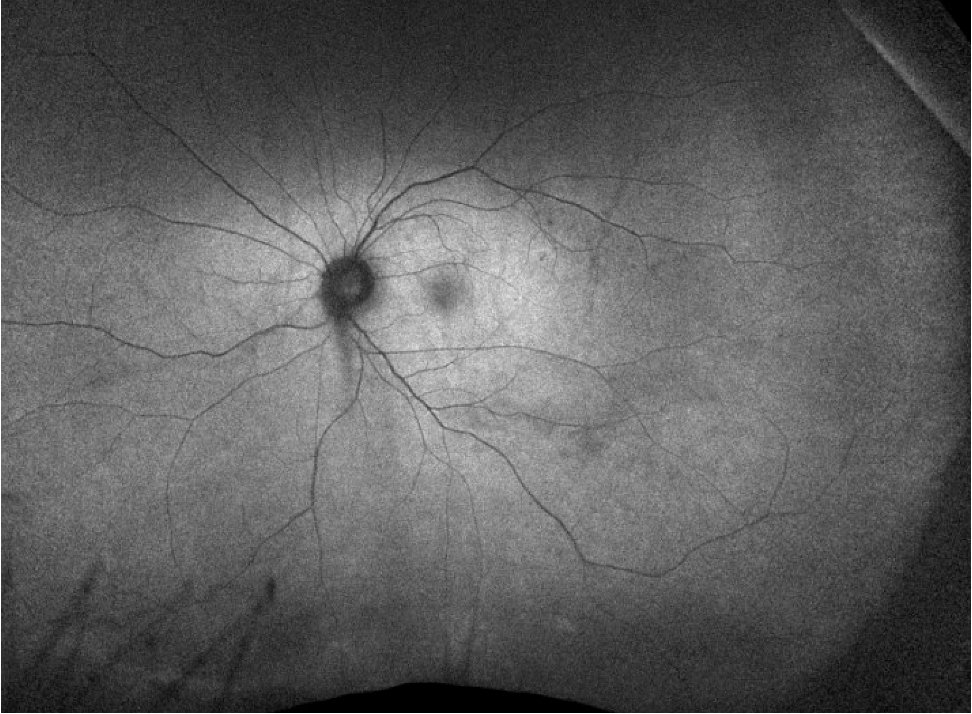
DFE
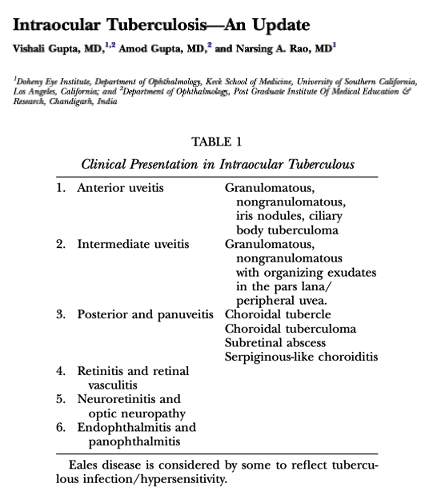
Differential Diagnosis
- For chorioretinitis or other white lesions in the retina
- Infectious:
- Toxoplasmosis
- Viral: CMV, HSV, rubella, West Nile virus
- HIV related eye diseases
- Tuberculosis
- Toxocara
- Syphilis
- Bartonella
- Fungal: Candida, Coccidioidomycosis, Presumed histoplasmosis
- Inflammatory:
- Sarcoidosis
- Behcets disease
- VKH
- White dot syndromes: MEWDS, APMPPE, Birdshot, Multifocal choroiditis and panuveitis, AZOOR, Punctate inner choroiditis, Serpiginous choroiditis
- Oncologic:
- Lymphoma
- Metastases
- CAR
- Melanoma
- Lymphoma
History
- Pt born in China
- 6/8: Ureteral stenting for renal papillary necrosis/gross hematuria
- 6/15: Admitted for postop recurrent fevers and perinephric hematoma
- Course c/b parainfluenza, ARDS
- 6/26: BAL revealed TB
- 6/30: Started on RIPE therapy
- 7/3: Inpatient ophthalmology evaluation, normal DFE
More History
- 7/30: steroids tapered off
- 8/7: ethambutol stopped
- Floaters and blurry vision started
- 8/30: pyrazinamide stopped as planned
- Pt continued on rifampin and isoniazid
Back to the Present (11/10)
- Patient sent from clinic to ED
- ID workup and management
- Workup for alternative etiologies
- Continued on pred and cyclo BID OS
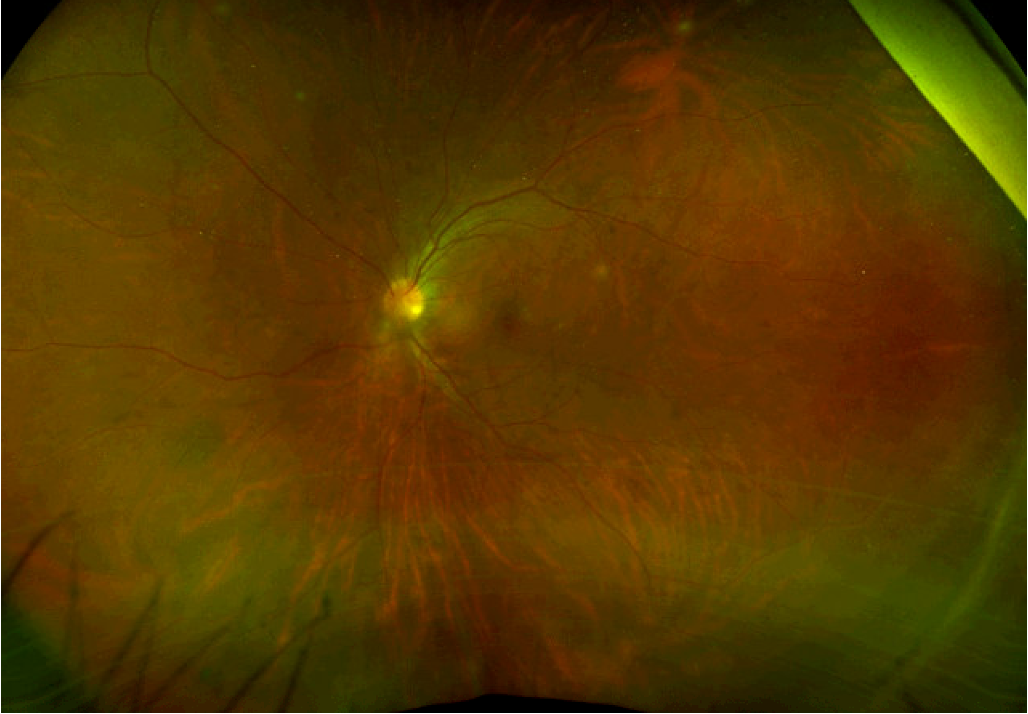
Workup
ID Management
- Discussion with DOH
- Continue RI
- Start moxifloxacin
- Start pyrazinamide
- Start bactrim
- Start prednisone
- Immune reconstitution inflammatory syndrome (IRIS)
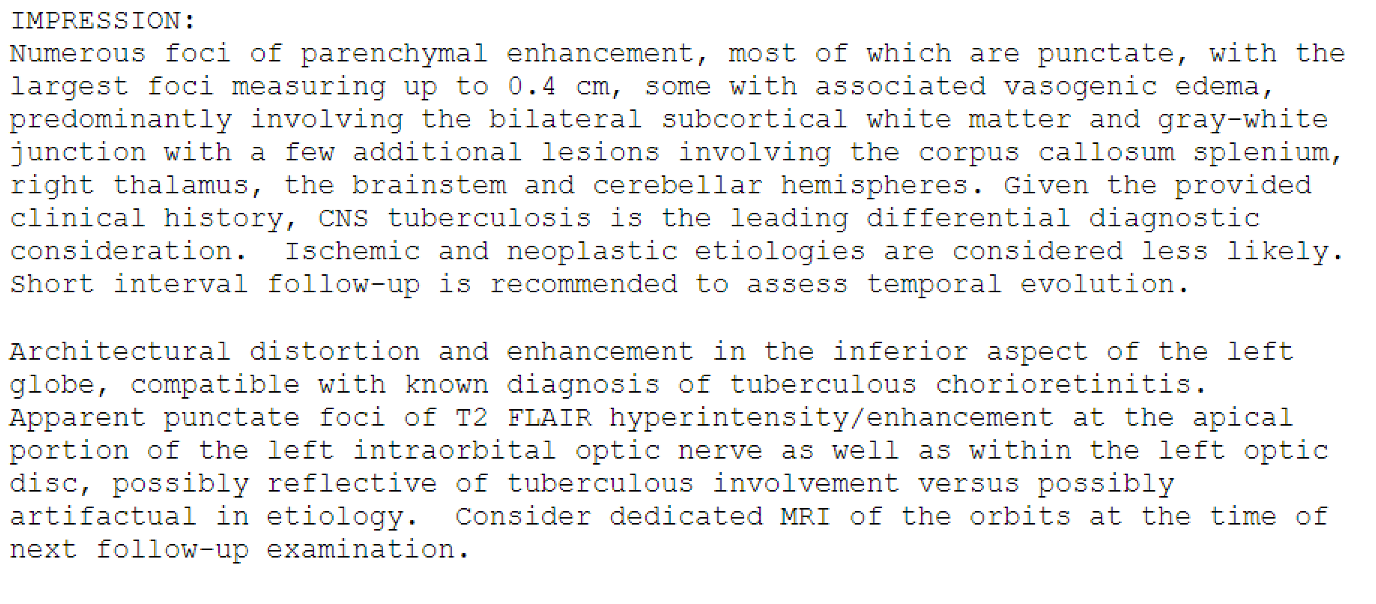
- MRI brain wwo
Discharge
- Patient stable on serial exams x 7 days
- Patient discharged for outpatient monitoring
- Patient followed closely on discharge
- Most recent visit on 11/27
Outpatient Follow-up (11/27)
VA 20/30, 20/30
Diagnosis
- Mycobacterium tuberculosis chorioretinitis of both eyes
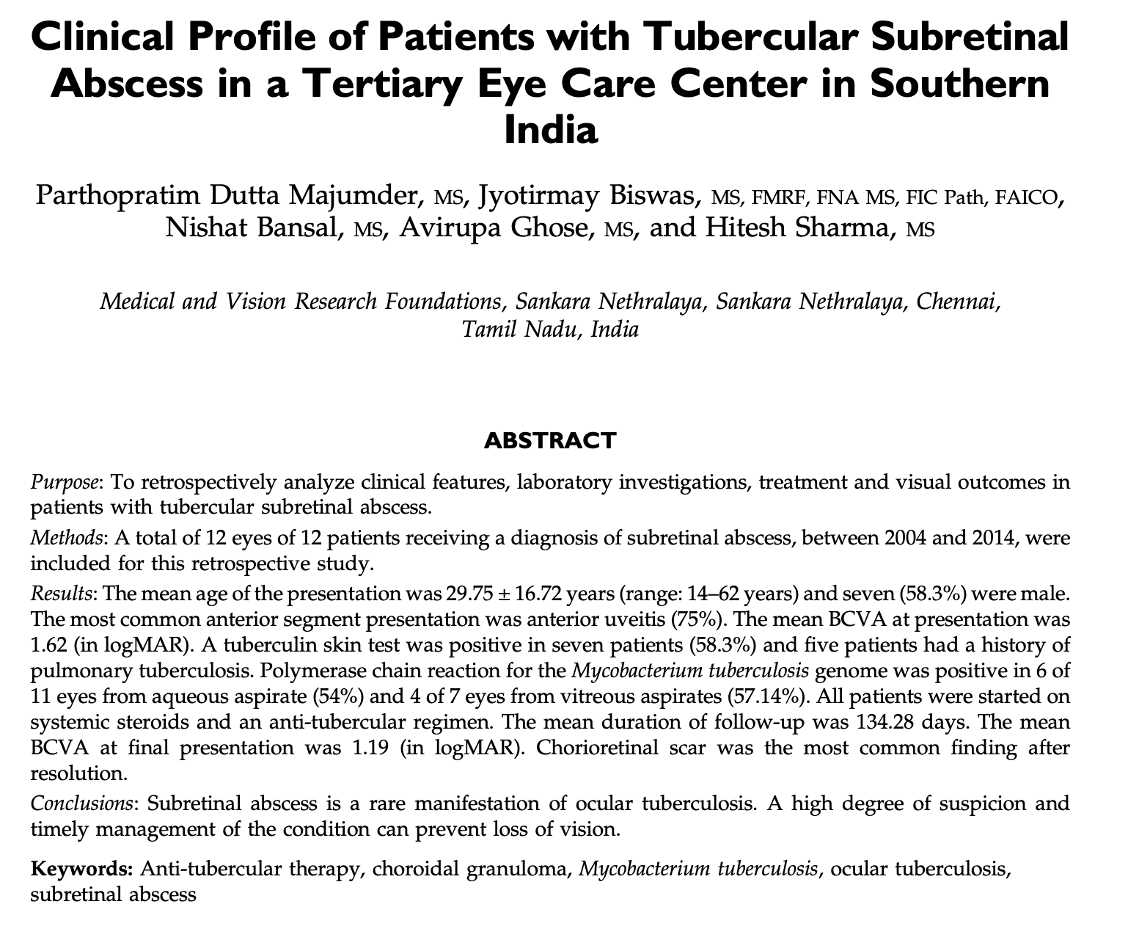
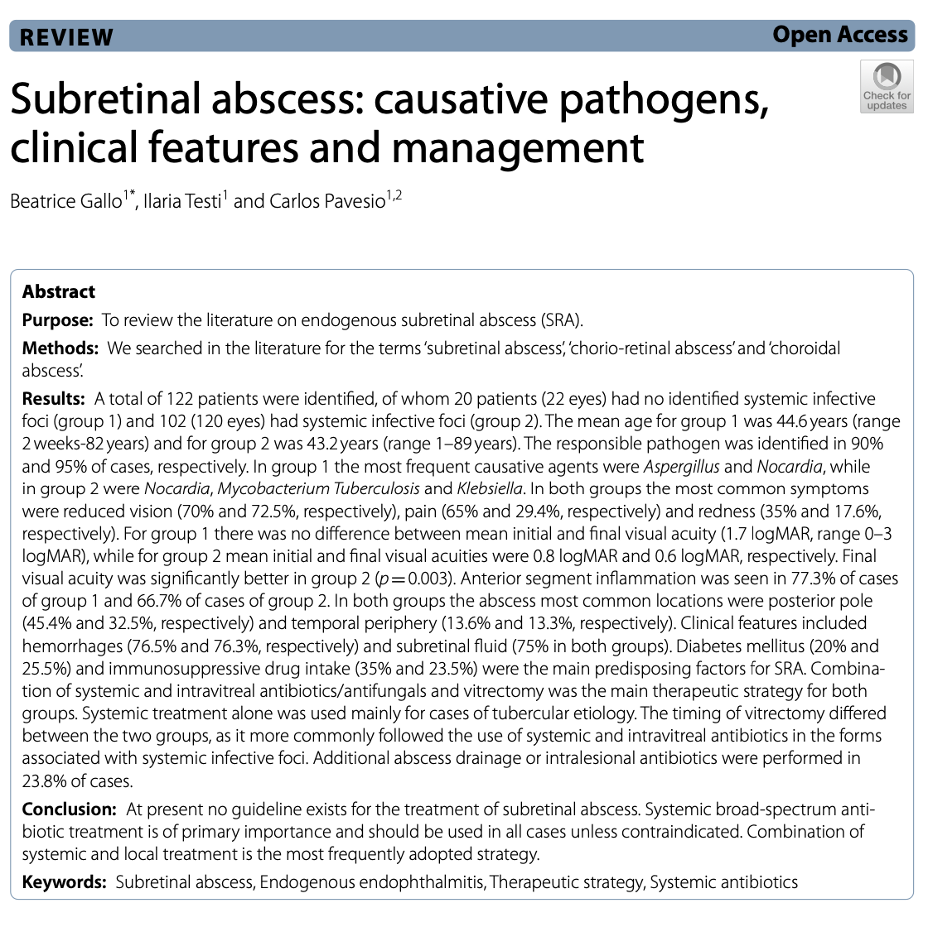
- Mycobacterial subretinal abscess of left eye
- Follow-up scheduled for 12/11/23
MRI Brain 12/2/23
Neuro-ophthalmology 12/7
- VA 20/40-2 ph 20/20-1, 20/40+2 ph NI
- HVF: Subtle inferior nasal defect OS
- Visual dysfunction likely 2/2 retinal findings
- MRI orbits without optic nerve infiltration or compressive lesion
Case Summary
- GU TB
- Ureteral stenting
- Hematogenous seeding
- Spread to lungs
- BAL w/TB
- Start on RIPE
- Taper to RI
- Ocular seeding
- Presentation to ophthalmology
- Admission
- Stable exams and TB therapy broadening
- Discharge
A Question for the Audience
- Should we suspect CNS involvement in patients with ocular TB?
- Chorioretinitis
- Subretinal abscess
Ocular TB Pearls
- Ocular involvement in 1-2% of TB cases
- Higher in endemic regions
- Hematogenous spread = most common
- Can be isolated to eye without systemic involvement
- Most typical lesions:
- choroidal granulomas
- occlusive retinal vasculitis
- multifocal serpiginous-like choroiditis
- Culture is gold standard, but rarely possible
- PCR used in some institutions
- Treatment is with systemic antitubercular drugs, often with steroids
158 patients between 1994-2004 seen in India
66 (42%) posterior uveitis
57 (36%) anterior uveitis
18 (11%) panuveitis
17 (11%) intermediate uveitis
- 354 patients
- Top three complications of intraocular tuberculosis:
- CME 107 (30%)
- Glaucoma 99 (28%)
- Cataract 71 (20%)