CASE OF THE MONTH: March 2022
A Patient with Vision Loss


History:
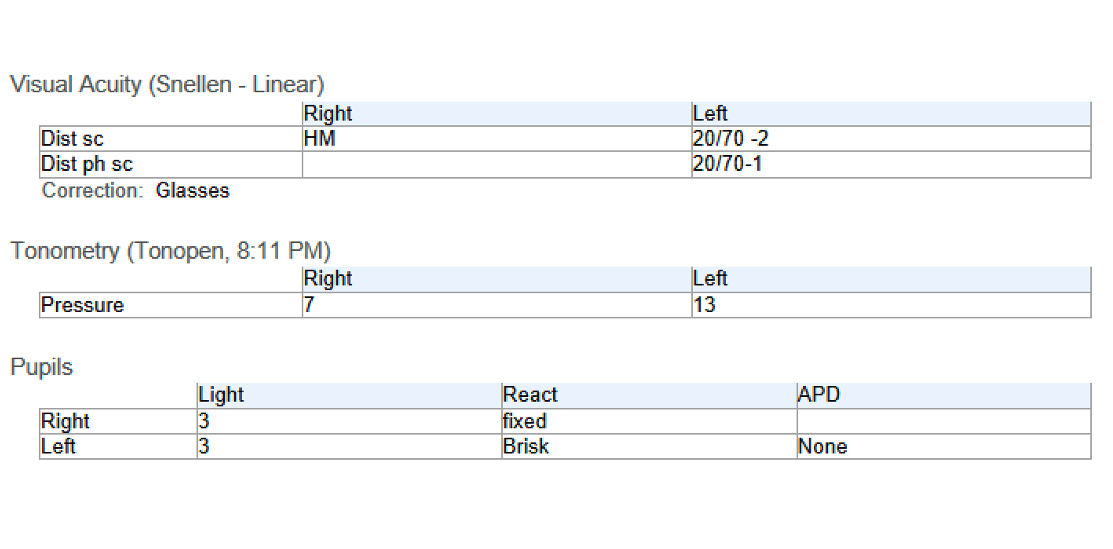
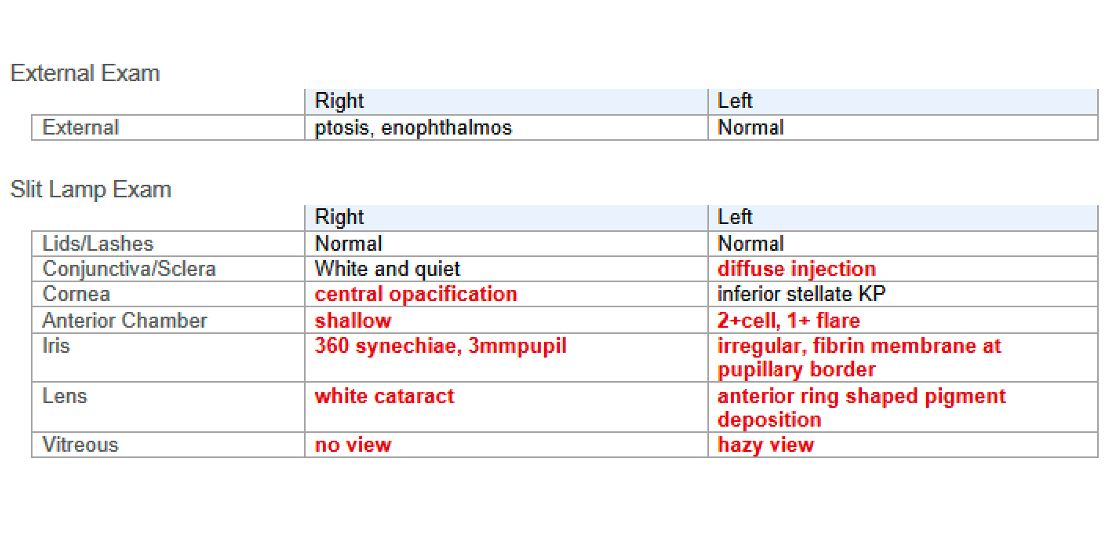
27-year-old male presents with redness, photophobia, and decreased vision OS x 2 days
PMH
- Cerebral palsy, epilepsy, encephalitis as an infant (etiology unknown)
POH:
- Trauma to OD at 3 years old, chronic HM vision (details unknown)
Social history:
- Lives in a group home
- No alcohol or drug use
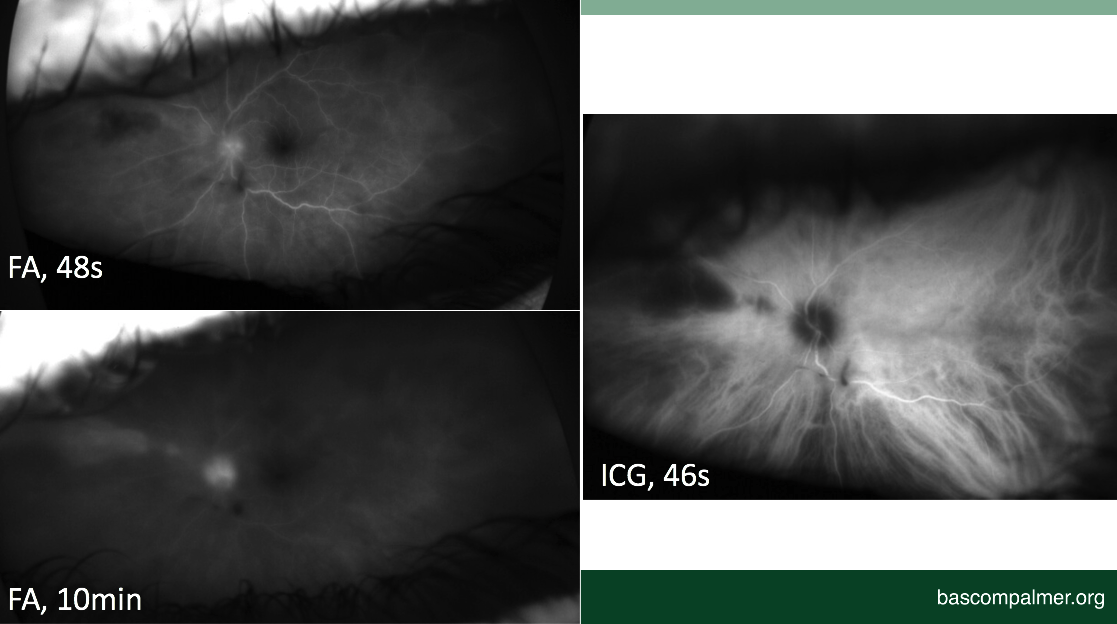
Exam
The case:
Differential Diagnosis:
- Infectious
- Acute Retinal Necrosis (ARN)
- Progressive Outer Retinal Necrosis (PORN)
- Cytomegalovirus (CMV) retinitis
- Syphilitic Retinitis
- Endophthalmitis
- Endogenous or exogenous
- Bacterial or fungal
- Toxoplasmosis
- Inflammatory
- Behcet's
- Sarcoidosi
- Sympathetic ophthalmia (trauma OD
- Vascular
- Arterial occlusion
- Neoplastic
- Lymphoma
- Leukemia
Work-Up
Serology:
- RPR/FTA
- ANCA
- HLA-B27
- Quantiferon
- CBC
- CMP
- HSV 1/2
- HIV
Anterior chamber tap:
- HSV 1/2
- VZV
- CMV
- Toxoplasmosis
Initial Management
- Valacyclovir 2g TID
- Intravitreal injection of foscarnet and ganciclovir (0.1 ml each)
- PF q2h OS, cyclopentolate TID OS
- Plan to start oral steroids if RPR & Quantiferon negative
Work-Up
Serology
- RPR/FTA - Negative
- ANCA - Negative
- HLA-B27 - Negative
- Quantiferon - Negative
- CBC - WNL
- CMP - WNL
- HSV 1/2 - HSV 2 IgG >8 (positive)
- HIV - Negative
Anterior chamber tap:
- HSV 1/2 - HSV 2 positive
- VZV - Negative
- CMV - Negative
- Toxoplasmosis - Negative
Diagnosis:
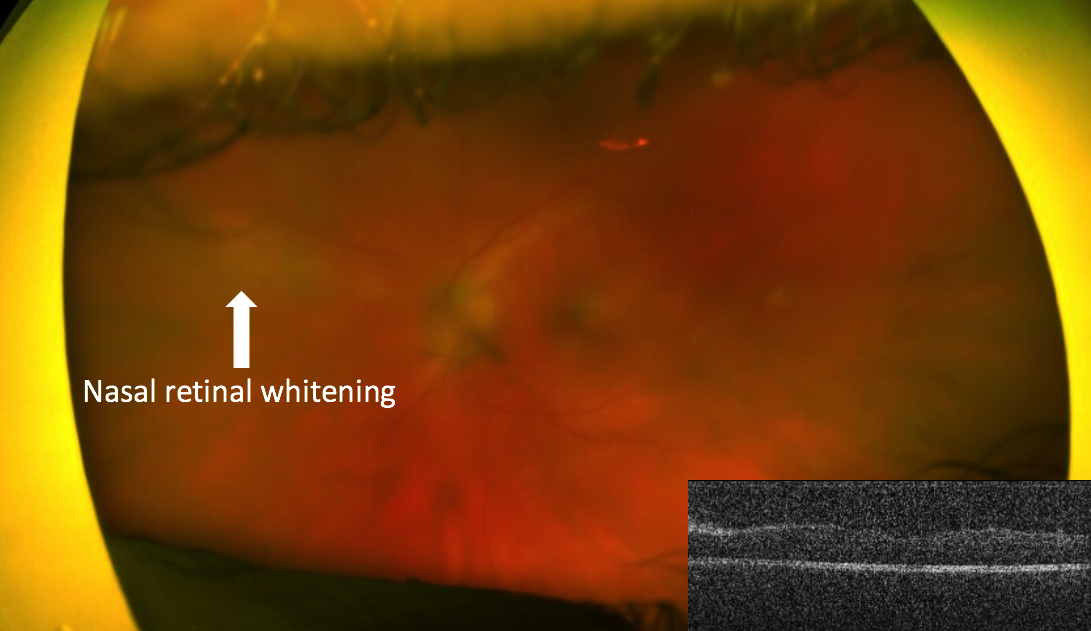
Acute Retinal Necrosis
Clinical Course:
- Given social issues at group home and monocular status, admitted to JMH for intravenous acyclovir 1g q8h and systemic steroids
- Course complicated by acute kidney injury and steroid psychosis, requiring temporary pause on antivirals
- Eventually re-started on IV acyclovir 500mg q8h, tolerated well
- Retinitis and uveitis improved
- After discharge, transitioned to PO valacyclovir 1g TID
History of ARN
1971: Urayama et al. first described unilateral acute uveitis with retinal periarteritis, necrotizing retinitis, and progression to retinal detachment
1978: Young & Bird coined the term acute retinal necrosis in a published series of 4 patients with similar findings
1. Urayama A, Yamada N, Sasaki T, et al. Unilateral acute uveitis with retinal periarteritis and detachment. Jpn J Clin Ophthalmol. 1971;25:607-619.
2. Young NJ, Bird AC. Bilateral acute retinal necrosis. Br J Ophthalmol. 1978 Sep;62(9):581-90. doi: 10.1136/bjo.62.9.581. PMID: 708676; PMCID: PMC1043304.
Etiology
1982: Culbertson et al. first reported histopathology and electron microscopy findings in an enucleated eye of a 67-year-old man with ARN
EM demonstrated herpes group virus in all layers of affected retina
1. Muthiah MN, Michaelides M, Child CS, et al. Acute retinal necrosis: a national population-based study to assess the incidence, methods of diagnosis, treatment strategies and outcomes in the UK. Br J Ophthalmol 2007;91:1452–5.
1. Muthiah MN, Michaelides M, Child CS, et al. Acute retinal necrosis: a national population-based study to assess the incidence, methods of diagnosis, treatment strategies and outcomes in the UK. Br J Ophthalmol 2007;91:1452–5.

1. Cochrane TF, Silvestri G, McDowell C, et al. Acute retinal necrosis in the United Kingdom: results of a prospective surveillance study. Eye (Lond). 2012;26:370-377.

1. Muthiah MN, Michaelides M, Child CS, et al. Acute retinal necrosis: a national population-based study to assess the incidence, methods of diagnosis, treatment strategies and outcomes in the UK. Br J Ophthalmol 2007;91:1452–5.
Clinical Features

1. Cochrane TF, Silvestri G, McDowell C, et al. Acute retinal necrosis in the United Kingdom: results of a prospective sur-veillance study. Eye (Lond). 2012;26:370-377.
2. Muthiah MN, Michaelides M, Child CS, et al. Acute retinal necrosis: a national population-based study to assess the incidence, methods of diagnosis, treatment strategies and outcomes in the UK. Br J Ophthalmol 2007;91:1452–5.
3. Holland GN. Executive Committee of the American Uveitis Society. Standard diagnostic criteria for the acute retinal necrosis syndrome. Am J Ophthalmol. 1994;117: 663–667.
4. Yannuzzi LA, et al. The Retinal Atlas. Second edition. [Philadelphia]: Elsevier, 2017.
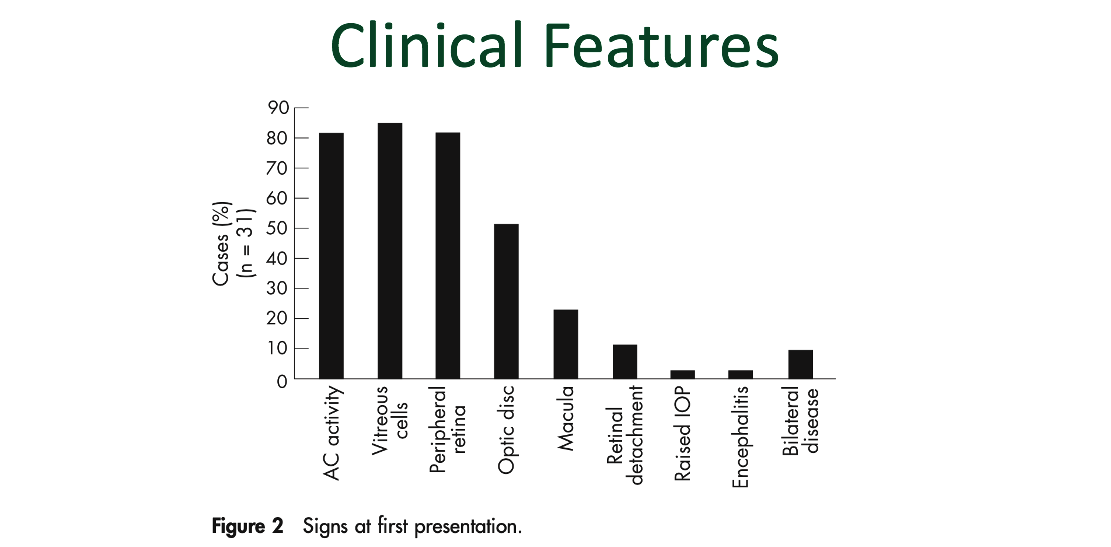
1. Muthiah MN, Michaelides M, Child CS, et al. Acute retinal necrosis: a national population-based study to assess the incidence, methods of diagnosis, treatment strategies and outcomes in the UK. Br J Ophthalmol 2007;91:1452–5.
- Late cicatricial phase
- Retinal atrophy
- Chorioretinal scarring
- Vascular nonperfusion
- Optic atrophy
- Epiretinal membrane
- Tractional and/or rhegmatogenous retinal detachment
1. Holland GN. Executive Committee of the American Uveitis Society. Standard diagnostic criteria for the acute retinal necrosis syndrome. Am J Ophthalmol. 1994;117: 663–667.
2. Chang S, Young LH. Acute retinal necrosis: an overview. Int Ophthalmol Clin 2007; 47(2)145–54
Diagnosis:
- ARN is a clinical diagnosis
- 1994 American Uveitis Society standard diagnostic criteria:
- (1) Well-demarcated areas of retinal necrosis in the peripheral retina
- (2) Rapid circumferential progression of retinal necrosis in absence of antivirals
- (3) Occlusive vasculopathy
- (4) Prominent inflammatory reaction in the anterior chamber and vitreous
- Diagnosis of ARN does not depend on immune status of host or isolation of pathogen
1. Holland GN. Executive Committee of the American Uveitis Society. Standard diagnostic criteria for the acute retinal necrosis syndrome. Am J Ophthalmol. 1994;117: 663–667.
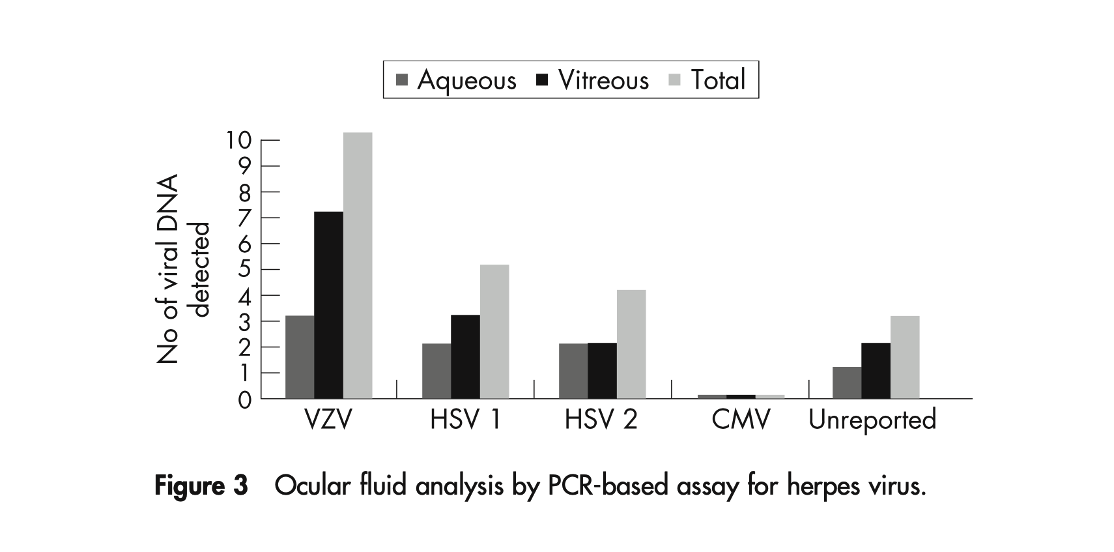
- Polymerase Chain Reaction
- PCR positive for HSV or VZV in 79% – 100% of cases of clinically suspected ARN
- Aqueous vs vitreous sample?
- Lack of data demonstrating superiority of one technique
- Do not wait for PCR results to initiate treatment if ARN is suspected
1. Cochrane TF, Silvestri G, McDowell C, et al. Acute retinal necrosis in the United Kingdom: results of a prospective sur- veillance study. Eye (Lond). 2012;26:370-377.
2. Schoenberger SD, Kim SJ, Thorne JE, et al. Diagnosis and Treatment of Acute Retinal Necrosis: A Report by the American Academy of Ophthalmology. Ophthalmology. 2017 Mar;124(3):382-392.
Treatment:
- Intravenous antivirals
- Historical standard of care
- 1986: Blumenkranz et al. reported regression of retinal lesions with intravenous acyclovir
- 1991: Palay et al. found reduction in contralateral involvement from 70% to 13% with intravenous acyclovir
1. Blumenkranz MS, Culbertson WW, Clarkson JG, Dix R. Treatment of the acute retinal necrosis syndrome with intra-venous acyclovir. Ophthalmology. 1986;93:296-300
2.. Palay DA, Sternberg Jr P, Davis J, et al. Decrease in the risk of bilateral acute retinal necrosis by acyclovir therapy. Am J Ophthalmol. 1991;112:250-255.
- Oral antivirals
- Advent of oral antivirals with greater bioavailability resulted in increased use of orals as first line therapy
- Outpatient administration, decreased cost
- Advent of oral antivirals with greater bioavailability resulted in increased use of orals as first line therapy
- Intravenous vs. oral?
- Comparable:
- Visual outcomes
- Incidence of retinal detachment
- Time to regression of retinitis
- Rates of contralateral eye involvement
- Comparable:
1. Schoenberger SD, Kim SJ, Thorne JE, et al. Diagnosis and Treatment of Acute Retinal Necrosis: A Report by the American Academy of Ophthalmology. Ophthalmology. 2017 Mar;124(3):382-392.
2. https://eyewiki.aao.org/Acute_Retinal_Necrosis#Medical_therapy
3. Baltinas J, Lightman S, Tomkins-Netzer O. Comparing Treatment of Acute Retinal Necrosis With Either Oral Valacyclovir or Intravenous Acyclovir. Am J Ophthalmol. 2018 Apr;188:173-180.
- Intravitreal antivirals
- Used with systemic medication, intravitreals provide immediate higher concentration in the eye than systemic treatment alone
1. Schoenberger SD, Kim SJ, Thorne JE, et al. Diagnosis and Treatment of Acute Retinal Necrosis: A Report by the American Academy of Ophthalmology. Ophthalmology. 2017 Mar;124(3):382-392.
Yeh S, Suhler EB, Smith JR, Bruce B, Fahle G, Bailey ST, Hwang TS, Stout JT, Lauer AK, Wilson DJ, Rosenbaum JT, Flaxel CJ. Combination systemic and intravitreal antiviral therapy in the management of acute retinal necrosis syndrome. Ophthalmic Surg Lasers Imaging Retina. 2014 Sep-Oct;45(5):399-407.
- Other adjuvant medical therapy
- Steroids:
- Topical:
- Commonly prescribed
- Oral:
- Often added 24-48 hours after antivirals to decrease severe inflammatory response1
- But no definitive benefit in the literature1
- » Tibbets et al. (Ophthalmology, 2010): 58 eyes, PO steroids not associated with improved VA
- » Lau et al. (Ophthalmology, 2007): 22 eyes; PO steroids not associated with RD
- Local (periocular, intravitreal):
- Can be used with caution, may potentiate progression of retinitis4
- Choudhury et al. (Can J Ophthalmol, 2014): 4 eyes
- » In eyes with persistent vitritis after treatment with systemic antivirals and steroids, intravitreal triamcinolone decreased vitritis and improved VA
- Topical:
- Steroids:
Shantha JG, Weissman HM, Debiec MR, Albini TA, Yeh S. Advances in the management of acute retinal necrosis. Int Ophthalmol Clin. 2015 Summer;55(3):1-13.
Tibbetts MD, Shah CP, Young LH et al. Treatment of acute retinal necrosis. Ophthalmology. 2010 Apr;117(4):818-24.
Lau CH, Missotten T, Salzmann J, Lightman SL. Acute retinal necrosis features, management, and outcomes. Ophthalmology. 2007 Apr;114(4):756-62.
Li AL, Fine HF, Shantha JG, Yeh S. Update on the Management of Acute Retinal Necrosis. Ophthalmic Surg Lasers Imaging Retina. 2019 Dec 1;50(12):748-751.
Choudhury H, Jindal A, Mithal K, et al. Intravitreal triamcinolone acetonide as an adjuvant in the management of acute retinal necrosis. Can J Ophthalmol. 2014;49(3):279-282.
Proposed treatment regimen:
1. Powell B, Wang D, Llop S, Rosen RB. Management Strategies of Acute Retinal Necrosis: Current Perspectives. Clin Ophthalmol. 2020 Jul 8;14:1931-1943.
2. Schlingemann RO, Bruinenberg M, Wertheim-van Dillen P, et al. Twenty years' delay of fellow eye involvement in herpes simplex virus type 2-associated bilateral acute retinal necrosis syndrome. Am J Ophthalmol. 1996;122:891–892.
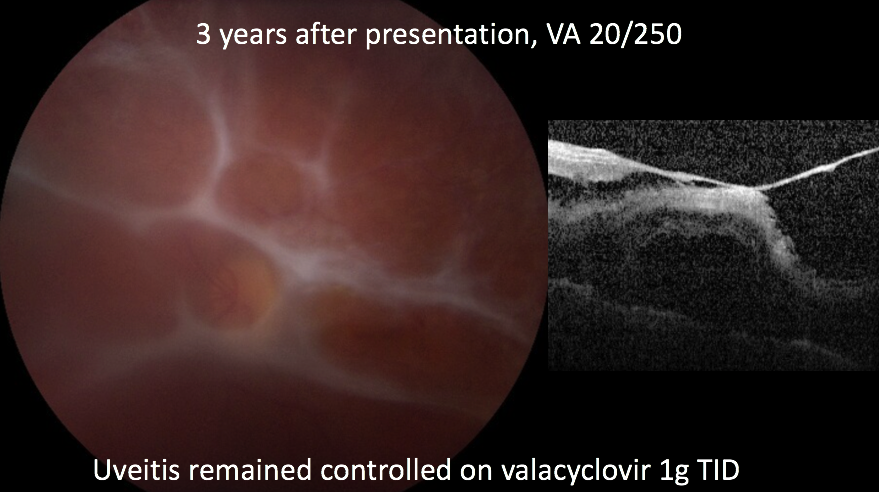
Our Patient – 2 months after presentation:
Clinical Course:
- 6 months after presentation, patient returned to ED with worsening vision OS
- VA decreased to 20/300
- Significant new anterior and posterior inflammation
- Received intravitreal foscarnet and ganciclovir, and re-admitted for IV acyclovir
- Inflammation improved, transitioned to valacyclovir 1g TID after discharge

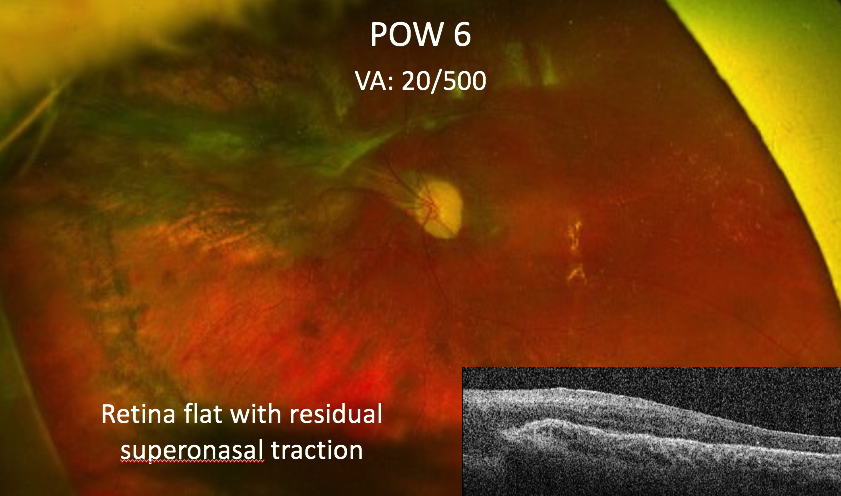
- 4 years after first presentation, patient presented to ED with 5 days of decreased vision
- VA decreased to HM
- Total retinal detachment
Retinal Detachment:
- Retinal Detachment in ARN
- High rates of occurrence, though reported rates vary widely (~ 20-73%)
- Usually occurs within 3 months of onset
- Large breaks at border of vital and ischemic retina
- Contraction of vitreous also contributes
- Often complicated by proliferative vitreoretinopathy (PVR)
- Contributes to poor visual outcomes
- Insufficient evidence to support the use of prophylactic laser or vitrectomy for retinal detachment prevention
1. Iwahashi-Shima C, Azumi A, Ohguro N, et al. Acute retinal necrosis: factors associated with anatomic and visual outcomes. Jpn J Ophthalmol. 2013
2. Chang S, Young LH. Acute retinal necrosis: an overview. Int Ophthalmol Clin 2007; 47(2)145–54
3. Schoenberger SD, Kim SJ, Thorne JE, et al. Diagnosis and Treatment of Acute Retinal Necrosis: A Report by the American Academy of Ophthalmology. Ophthalmology. 2017 Mar;124(3):382-392.
Visual Prognosis:
- Visual prognosis is poor, even with appropriate treatment
- Cochrane et al. (Eye, 2012): 52 eyes
- 48% have VA of ❬20/200 six months after onset
- Baltinas et al. (AJO, 2018): 68 eyes
- 51% had severe vision loss (❬20/200)
- Tibbets et al. (Ophthalmology, 2010): 58 eyes
- 50% had VA of 20/200 or worse by 3 months, 75% by 5 years
- Cochrane et al. (Eye, 2012): 52 eyes
- Mechanisms of vision loss: Retinal detachment, chronic vitritis, epiretinal membrane, macular ischemia, macular edema, optic neuropathy
- Systemic morbidity and mortality associated with CNS involvement
1. Cochrane TF, Silvestri G, McDowell C, et al. Acute retinal necrosis in the United Kingdom: results of a prospective sur- veillance study. Eye (Lond). 2012;26:370-377.
2. Baltinas J, Lightman S, Tomkins-Netzer O. Comparing Treatment of Acute Retinal Necrosis With Either Oral Valacyclovir or Intravenous Acyclovir. Am J Ophthalmol. 2018 Apr;188:173-180.
3. Tibbetts MD, Shah CP, Young LH et al. Treatment of acute retinal necrosis. Ophthalmology. 2010 Apr;117(4):818-24.
4. Schoenberger SD, Kim SJ, Thorne JE, et al. Diagnosis and Treatment of Acute Retinal Necrosis: A Report by the American Academy of Ophthalmology. Ophthalmology. 2017 Mar;124(3):382-392.
Summary:
- • Acute retinal necrosis is a rare viral retinitis most commonly caused by VZV, followed by HSV 1 or 2
- • Prompt initiation of antivirals is critical
- Can use intravenous or oral antivirals
- Combination therapy with intravitreal antivirals appears to improve outcomes
- • Retinal detachment is a common complication
- Role for prophylactic laser or early vitrectomy remains unclear
- Visual prognosis is guarded