CASE OF THE MONTH: December 2021
Superior scotoma and flashes in a young myope


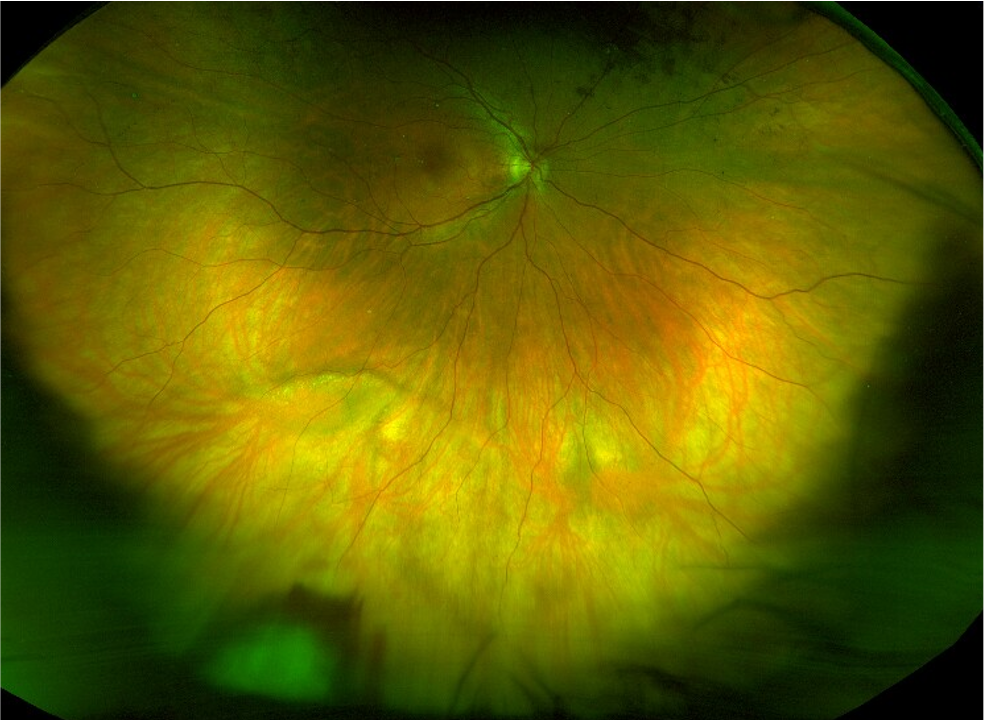
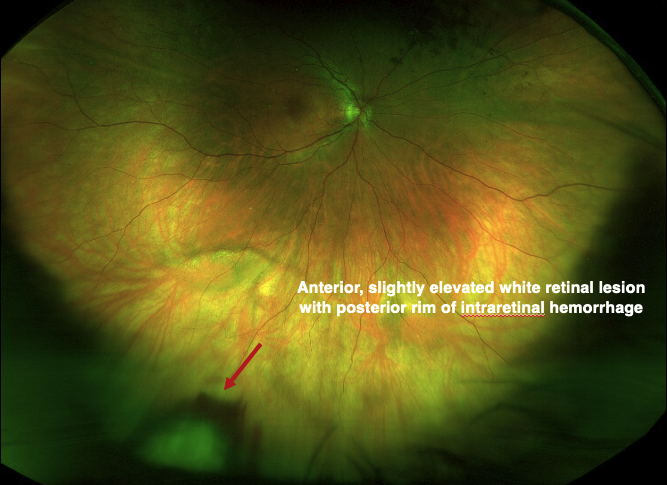
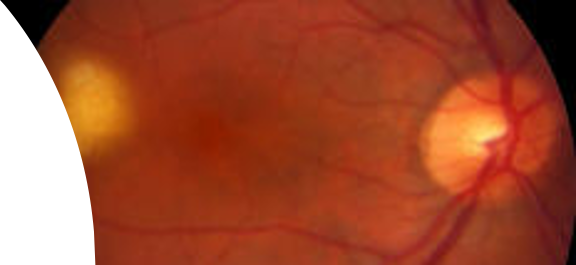
- 37 year-old female presents with history of six weeks of a “spot” in her superotemporal visual field with flashes in the right eye
- At presentation, she has been asymptomatic for one week
History:
- Past medical history: Hashimoto’s disease, shingles (fall 2020)
- Past ocular history: myopic LASIK (2010)
- Social history: Never smoker
- Family history: None
Exam:
- Visual acuity: 20/20-1 OU
- IOP: 15, 14
- Pupils: No RAPD
- Anterior segment: Unremarkable OU


Differential Diagnosis:
- White retinal lesion
- Retinal necrosis
- History of Zoster in 2020
- No current lesions
- No other systemic symptoms

- Primary vitreoretinal lymphoma
- Denies fevers, chills, weight loss
- Infectious/inflammatory lesions
- Tuberculoma
- No risk factors, no relevant travel history
- Denies systemic symptoms
- Sarcoid granuloma
- Denies related systemic symptoms
- Tuberculoma

- Retinal capillary hemangioma
- Von Hippel-Lindau
- No family history
- No systemic associations
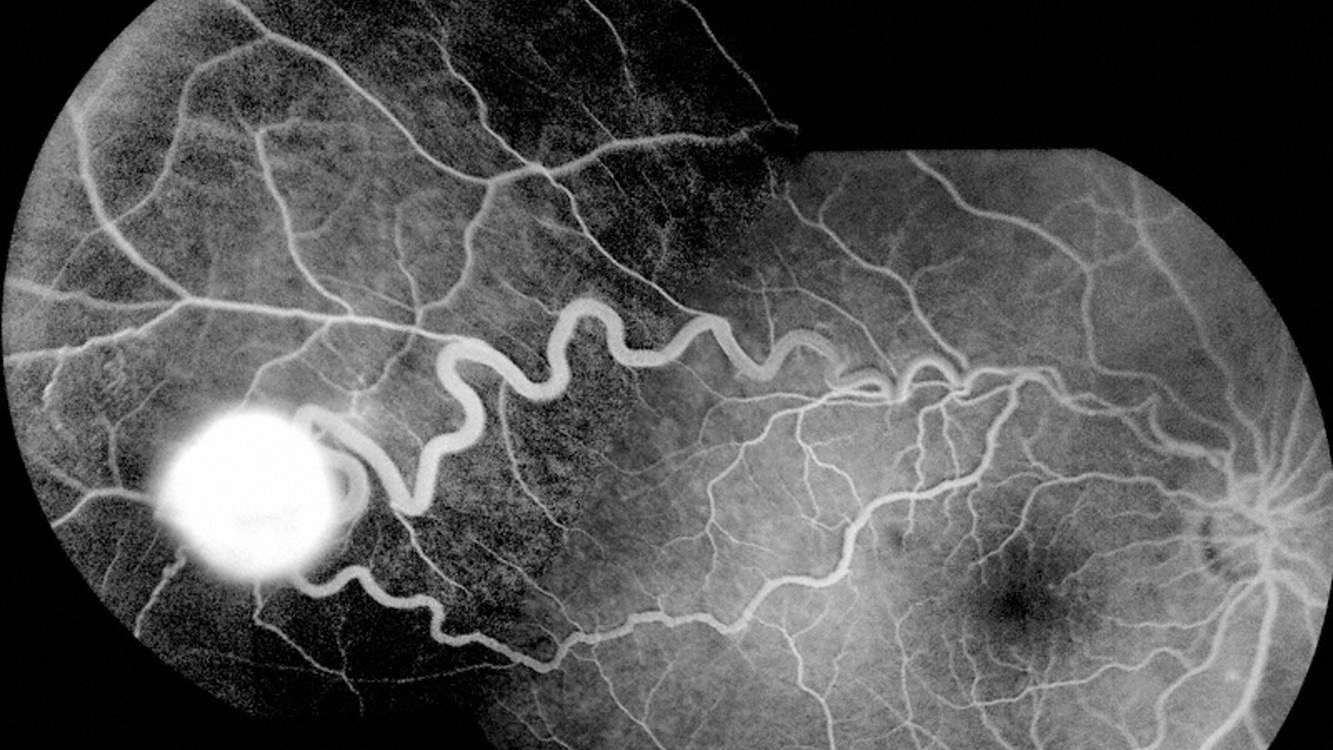
- Absence of markedly dilated and tortuous feeder vessels
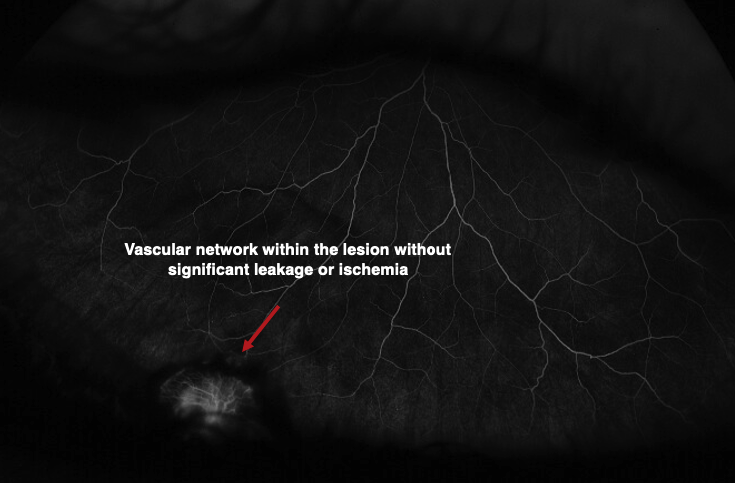
- Lacks characteristic angiographic appearance of marked hyperfluroescence of entire tumor
- Von Hippel-Lindau
- Amelanotic melanoma
- Choroidal
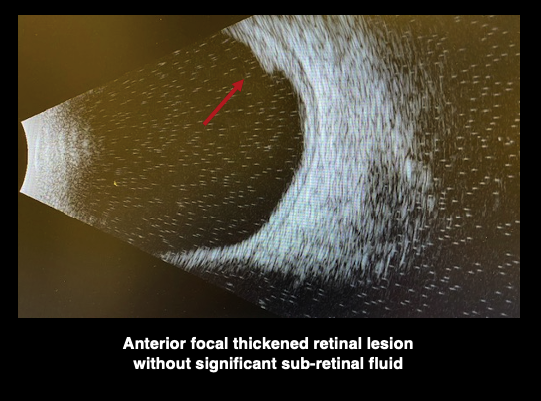
- B-scan low and decreasing internal reflectivity with choroidal shadowing
- Choroidal
- Peripheral exudative hemorrhagic chorioretinopathy
- Associated with large subretinal hemorrhage and exudate
- Lack telangiectatic feeder vessels
- Older patients

Diagnosis:
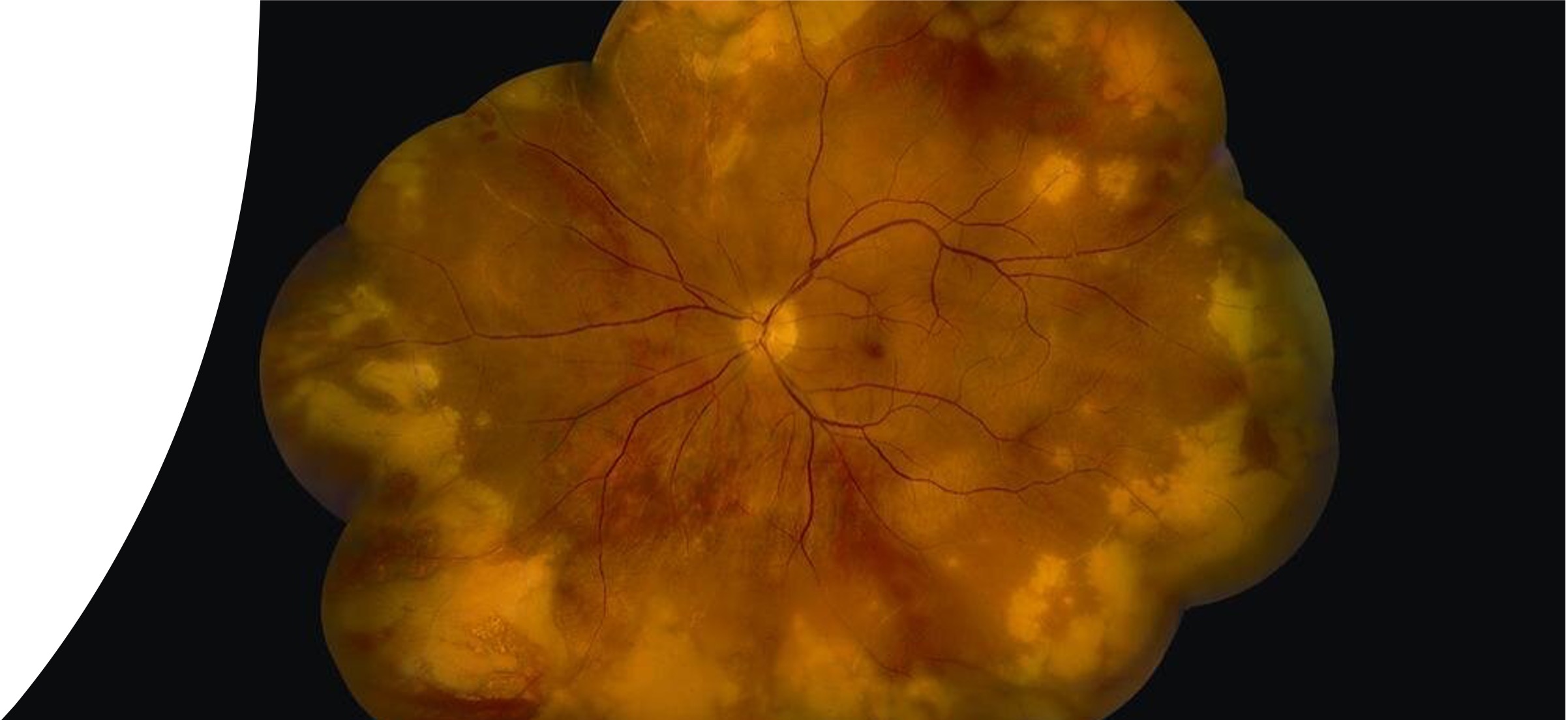
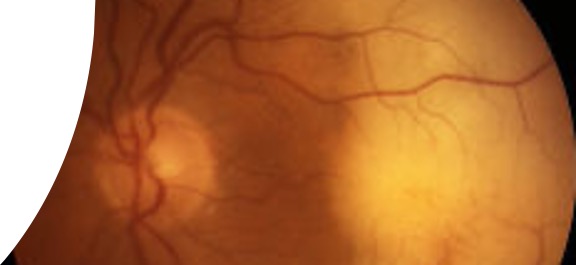
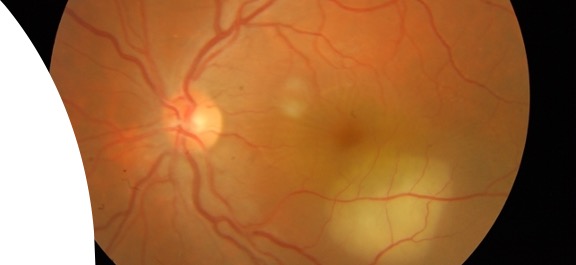
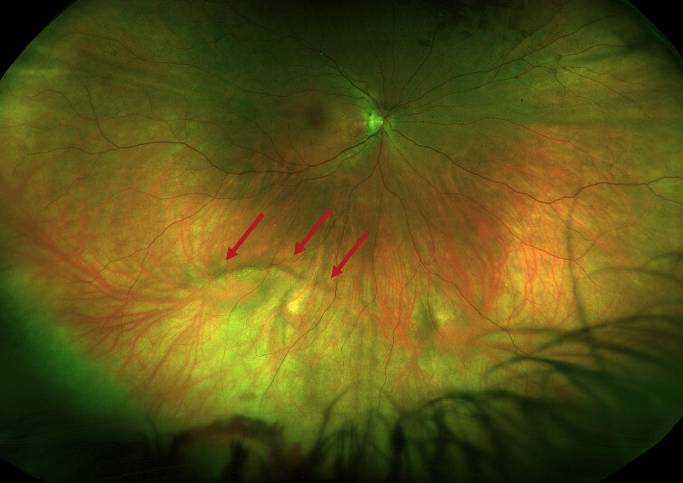
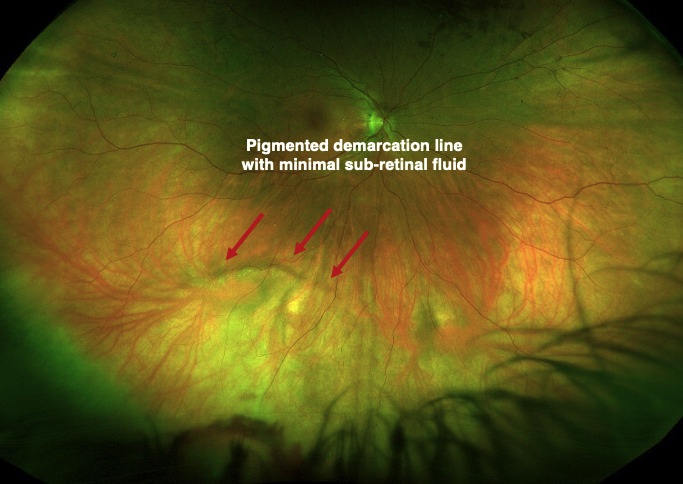
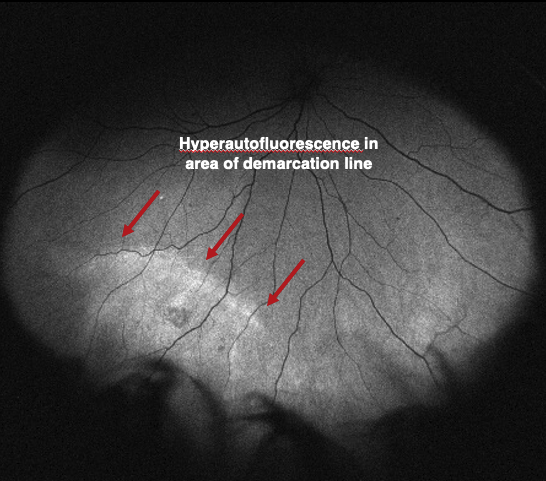
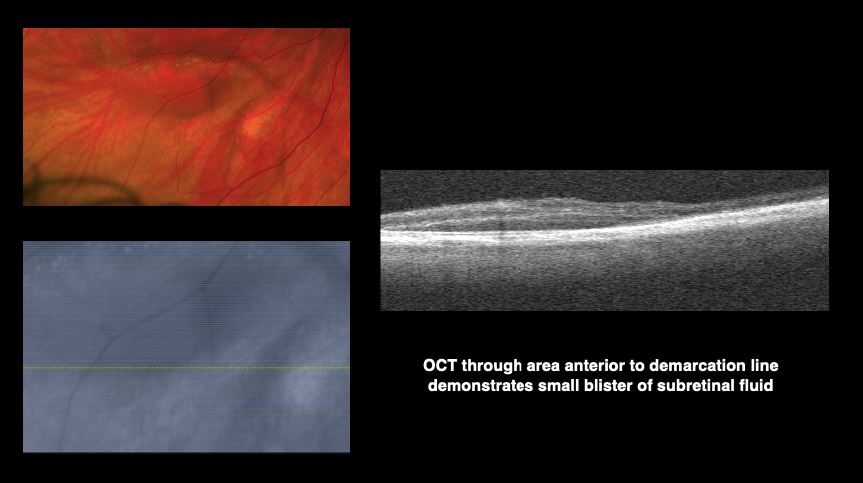
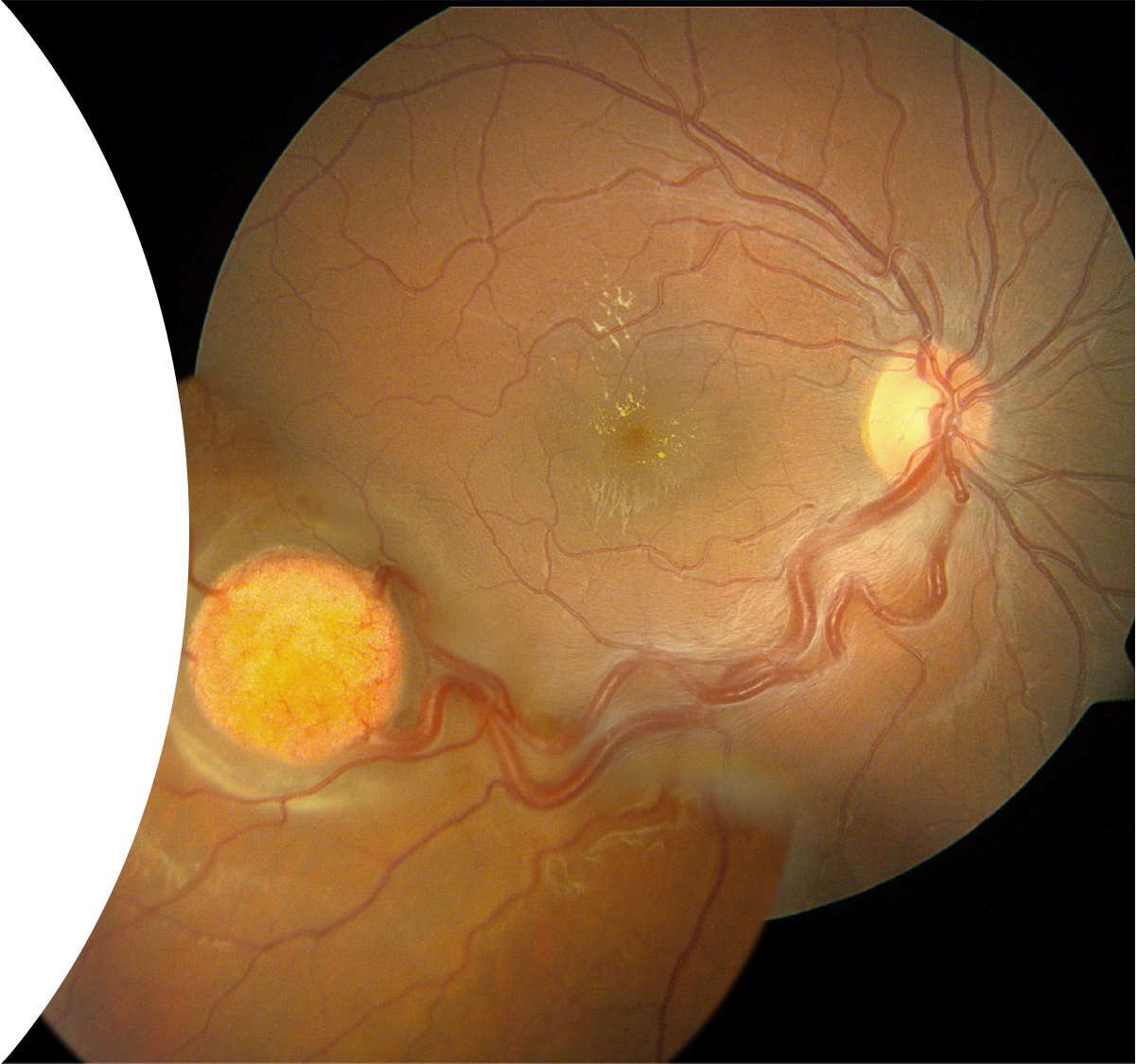
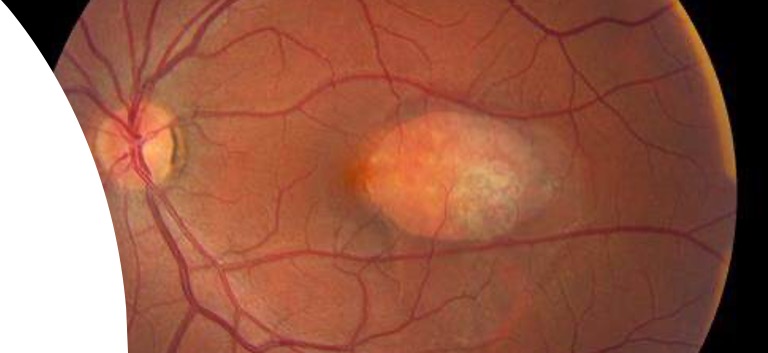
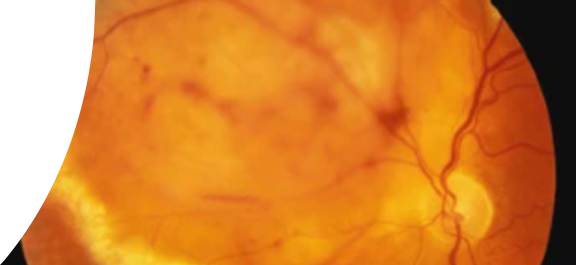
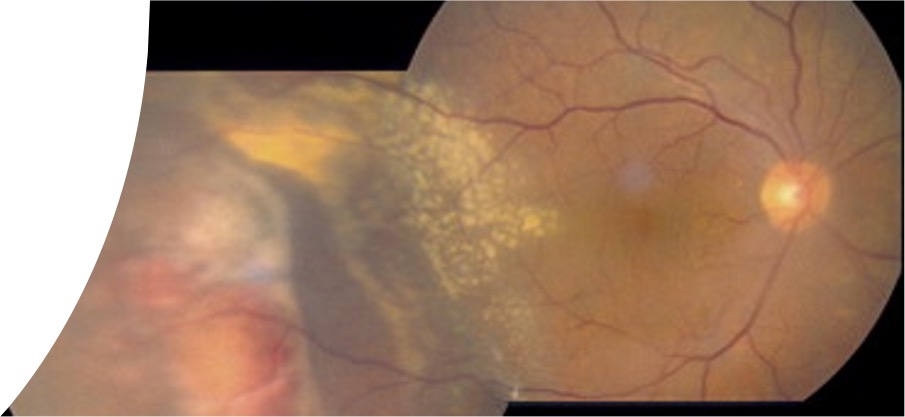
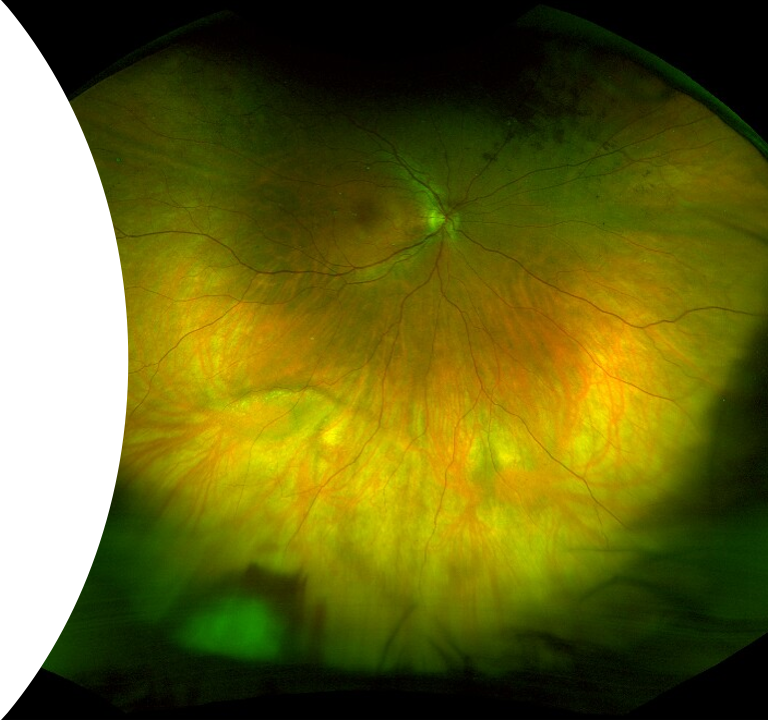
Retinal Vasoproliferative Tumor (VPT) with (receding) associated exudative retinal detachment
- Uncommon, benign, yellow-pink, dome-shaped retinal tumors with an overlying network of fine, telangiectatic vessels
- Primarily located inferotemporally or inferiorly in the retina
- May be isolated (primary) or associated with underlying ocular condition (secondary)
- Associated exudation, macular edema, retinal detachments, and epiretinal membranes can result in decreased vision
Treatment Modalities:
- Observation
- Appropriate for small, peripheral tumors that do not compromise vision
- Laser photocoagulation
- Useful for small tumors, usually as complement to other modalities
- Trans-scleral cryotherapy
- May induce tumor regression
- Adverse effects include macular edema, retinal detachment
- Photodynamic therapy/Transpupillary thermotherapy
- Useful in inducing regression for tumors of moderate thickness
- Brachytherapy
- Indicated for large lesions and those associated with retinal detachment
- Adverse effects include dry eye, cataract, optic neuropathy/retinopathy, neovascular glaucoma
- Surgical resection
- Indicated when tumors fail to respond to cryotherapy or in cases with persistent vitreous hemorrhage
- Intravitreal anti-VEGF
- Associated with temporary reduction in tumor thickness but have limited efficacy as long-term monotherapy
Back to our case:
- Patient offered: observation, cryotherapy, trans-pupillary thermotherapy
- Plan: Observation, avoid blood thinners and vigorous activity
- Five months later: Heme resolved, lesion inactive without recurrent exudation (and resolved SRF), observed
References:
Anastassiou G, Bornfeld N, Schueler AO, et al. Ruthenium-106 plaque brachytherapy for symptomatic vasoproliferative tumours of the retina. Br J Ophthalmol 2006;90:447–450.
Blasi MA, Scupola A, Tiberti AC, et al. Photodynamic therapy for vasoproliferative retinal tumors. Retina 2006;26:404–409.
Brockmann C, Rehak M, Heufelder J, et al. Predictors of treatment response of vasoproliferative retinal tumors to ruthenium-106 brachytherapy. Retina 2016;36:2384–2390.
Chan RPS, Lai TYY. Photodynamic therapy with verteporfin for vasoproliferative tumour of the retina. Acta Ophthalmol 2010;88:711–712.
Cohen VML, Shields CL, Demirci H, Shields JA. Iodine I 125 plaque radiotherapy for vasoproliferative tumors of the retina in 30 eyes. Arch Ophthalmol 2008;126:1245–1251.
Collaer N, James C. Vasoproliferative tumor of the retina in association with spontaneously reattached rhegmatogenous retinal detachment. Retin Cases Br Rep 2008;2:278–279.
Damato B. Vasoproliferative retinal tumour B. Br J Ophthalmol 2006;90:399–400.
Fujiya A, Noda K, Yoshida S, et al. Increased vascular endothelial growth factor level in the subretinal fluid of eye with vasoproliferative retinal tumors. Retin Cases Br Reports 2015;9:154–156.
Garcia-Arumi J, Distefano LN, Fonollosa A, et al. Management of Vision-Threatening Complications of Vasoproliferative Tumors of the Retina. Ophthalmic Res 2015;54:34–40.
Grossniklaus HE, Lenis TL, Jakobiec FA. Retinal Reactive Astrocytic Tumor (Focal Nodular Gliosis): The Entity Also Known as Vasoproliferative Tumor. Ocul Oncol Pathol 2017;3:161–163.
Heimann H, Jmor F, Damato B. Imaging of retinal and choroidal vascular tumours. Eye 2013;27:208–216.
Henkind P, Morgan G. Peripheral Retinal Angioma with Exudative Retinopathy In Adults (Coats’s Lesion). Brit J Ophthal 1966;50:2–12.
Hiscott P, Mudhar H. Is vasoproliferative tumour (reactive retinal glioangiosis) part of the spectrum of proliferative vitreoretinopathy? Eye 2009;23:1851–1858.
Huang Y-M, Chen S-J. Clinical characters and treatments of retinal vasoproliferative tumors. Taiwan J Ophthalmol 2016;6:85–88.
Hudson LE, Mendoza PR, Yan J, Grossniklaus HE. Reactive Retinal Astrocytic Tumor (Focal Nodular Gliosis): A Case Report. Ocul Oncol Pathol 2017;3:1–7.
Hussain RN, Jmor F, Damato B, Heimann H. Verteporfin Photodynamic Therapy for the Treatment of Retinal Vasoproliferative Tumors. Ophthalmology 2015;122:2361–2363.
Jakobiec FA, Thanos A, Stagner AM, et al. So-called massive retinal gliosis: A critical review and reappraisal. Surv Ophthalmol 2016;61:339–356.
Krivosic V, Massin P, Desjardins L, et al. Management of idiopathic retinal vasoproliferative tumors by slit-lamp laser or endolaser photocoagulation. Am J Ophthalmol 2014;158:154–161.
Marback EF, Guerra RL, Maia Junior O de O, Marback RL. Retinal vasoproliferative tumor. Arq Bras Oftalmol 2013;76:200–203.
Nickerson SJ, Al-Dahmash SA, Shields CL, Shields JA. Retinal vasoproliferative tumor with total retinal detachment managed with plaque radiotherapy. Oman J Ophthalmol 2012;5:53–54.
Nomura Y, Tamaki Y, Tsuji H, et al. Transpupillary thermotherapy for vasoproliferative retinal tumor. Retin Cases Br Reports 2009;3:358–360.
Para Prieto M, Saornil MA, de Frutos Baraja JM, et al. Episcleral brachytherapy as an effective alternative in vasoproliferative tumors. Int J Ophthalmol 2018;11:2017–2020.
Poole Perry LJ, Jakobiec FA, Zakka FR, et al. Reactive retinal astrocytic tumors (so-called vasoproliferative tumors): histopathologic, immunohistochemical, and genetic studies of four cases. Am J Ophthalmol 2013;155:593–608.
Rennie IG. Retinal vasoproliferative tumours. Eye 2010;24:468–471.
Rogers C, Damato B, Kumar I, Heimann H. Intravitreal bevacizumab in the treatment of vasoproliferative retinal tumours. Eye 2014;28:968–973.
Saito W, Kase S, Fujiya A, et al. Expression of vascular endothelial growth factor and intravitreal anti-vegf therapy with bevacizumab in vasoproliferative retinal tumors. Retina 2013;33:1959–1967.
Saldanha MJ, Edrich C. Treatment of vasoproliferative tumors with photodynamic therapy. Ophthalmic Surg Lasers Imaging 2008;39:143–145.
Singh AD, Soto H, Bellerive C, Biscotti C V. Reactive Retinal Astrocytic Tumor (Focal Nodular Gliosis): Report of the Clinical Spectrum of 3 Cases. Ocul Oncol Pathol 2017;3:235–239.
Shankar P, Bradshaw SE, Ang A, et al. Vascularised epiretinal membrane associated with vasoproliferative tumour [5]. Eye 2007;21:1003–1004.
Shields CL, Shields JA, Barrett J, Potter P De. Vasoproliferative Tumors of the Ocular Fundus. Arch Ophthalmol 1995;113:615–623.
Shields CL, Kaliki S, Al-Dahmash S, et al. Retinal vasoproliferative tumors: Comparative clinical features of primary vs secondary tumors in 334 cases. JAMA Ophthalmol 2013;131:328–334.
Shields JA, Reichstein D, Mashayekhi A, Shields CL. Retinal vasoproliferative tumors in ocular conditions of childhood. J AAPOS 2012;16:6–9.
Shields JA, Decker WL, Sanborn GE, et al. Presumed Acquired Retinal Hemangiomas. Ophthalmology 1983;90:1292–1300.
Shields JA, Shields CL. Reactive retinal astrocytic tumors (so-called vasoproliferative tumors): Histopathologic, immunohistochemical, and genetic studies of four cases. Am J Ophthalmol 2013;156:202–203.
Smith J, Steel D. The surgical management of vasoproliferative tumours. Ophthalmologica 2011;226 Suppl:42–45.
Temblador-Barba I, Delgado-Alonso EM, Toribio-García M, et al. Update on the management of vasoproliferative tumour. Arch Soc Esp Oftalmol 2018;93:350–353.
Wang Q, Day S, Nixon PA, Wong RW. Combined rhegmatogenous and traction detachment associated with vasoproliferative tumor secondary to sickle cell retinopathy. Am J Ophthalmol Case Rep 2016;4:4–6.
Yeh S, Wilson DJ. Pars plana vitrectomy and endoresection of a retinal vasoproliferative tumor. Arch Ophthalmol 2010;128:1196–1199.
Zheng B, Chen Y, Chen L, et al. Comparative Study on the Efficacy and Safety of Tumor Resection in Vitrectomy for Retinal Vasoproliferative Tumors. J Ophthalmol 2019;2019:7464123.