CASE OF THE MONTH: November 2024
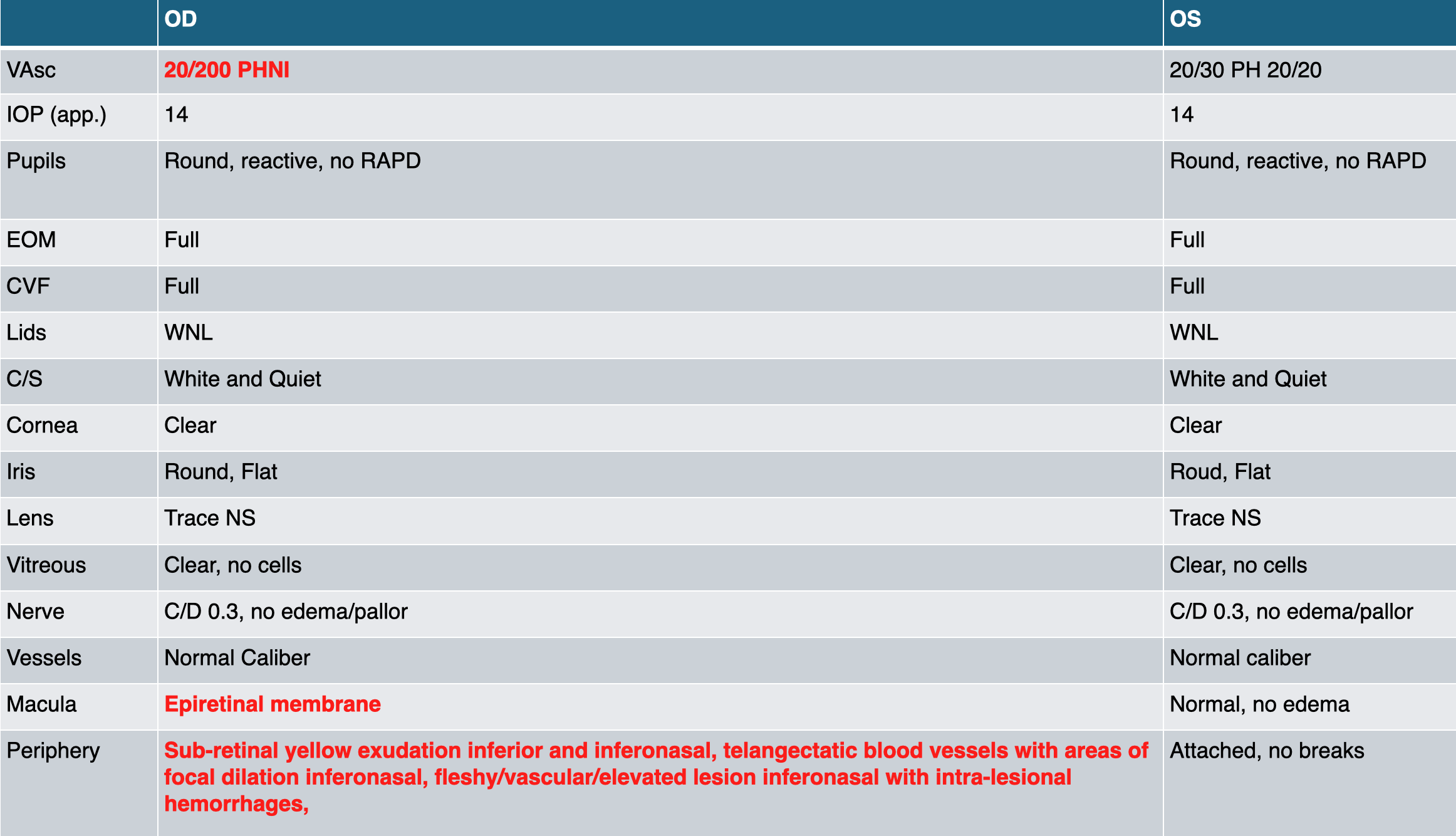
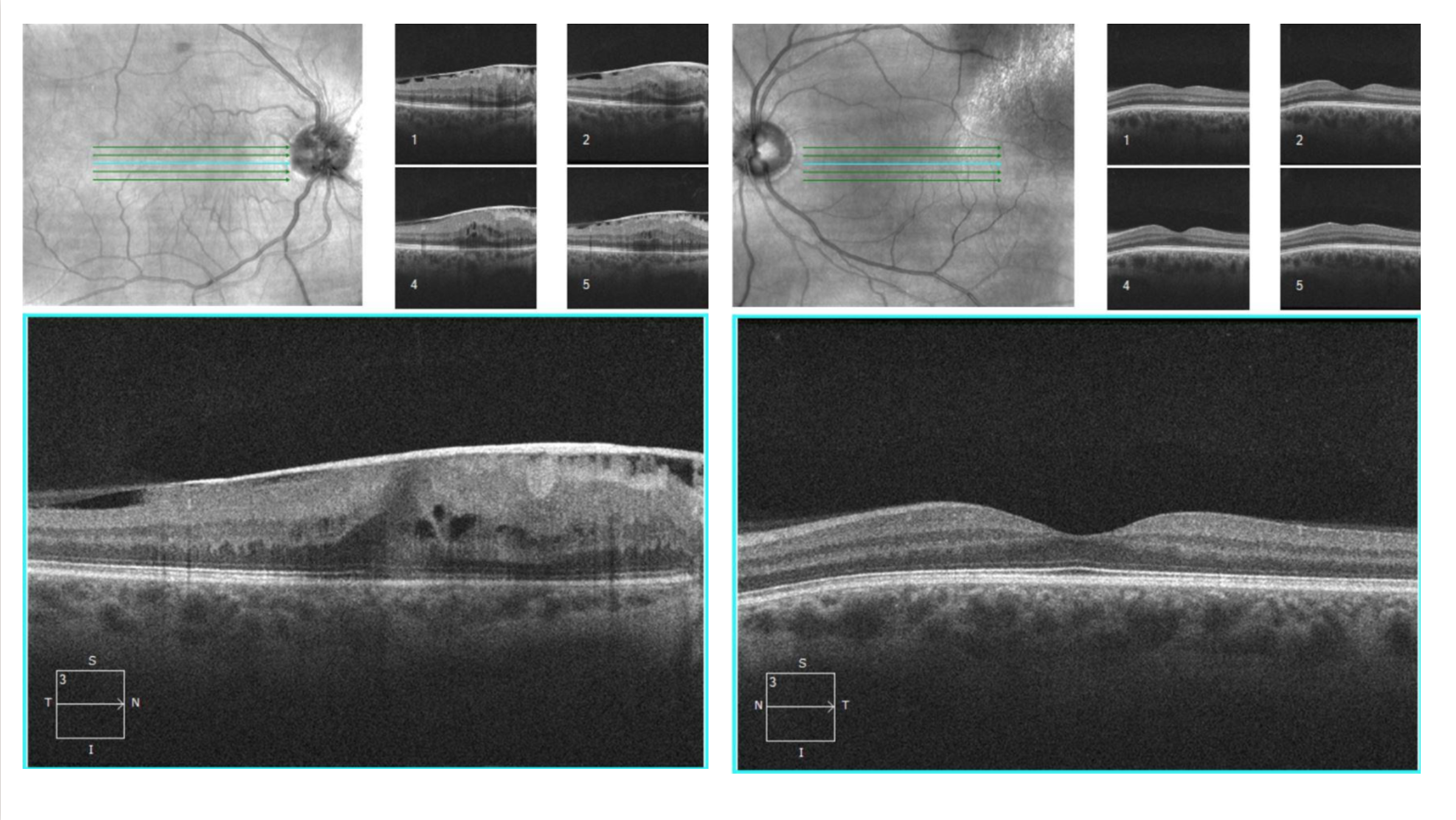
Self-peeling ERM in the Setting of a PARG Lesion

Presentation:
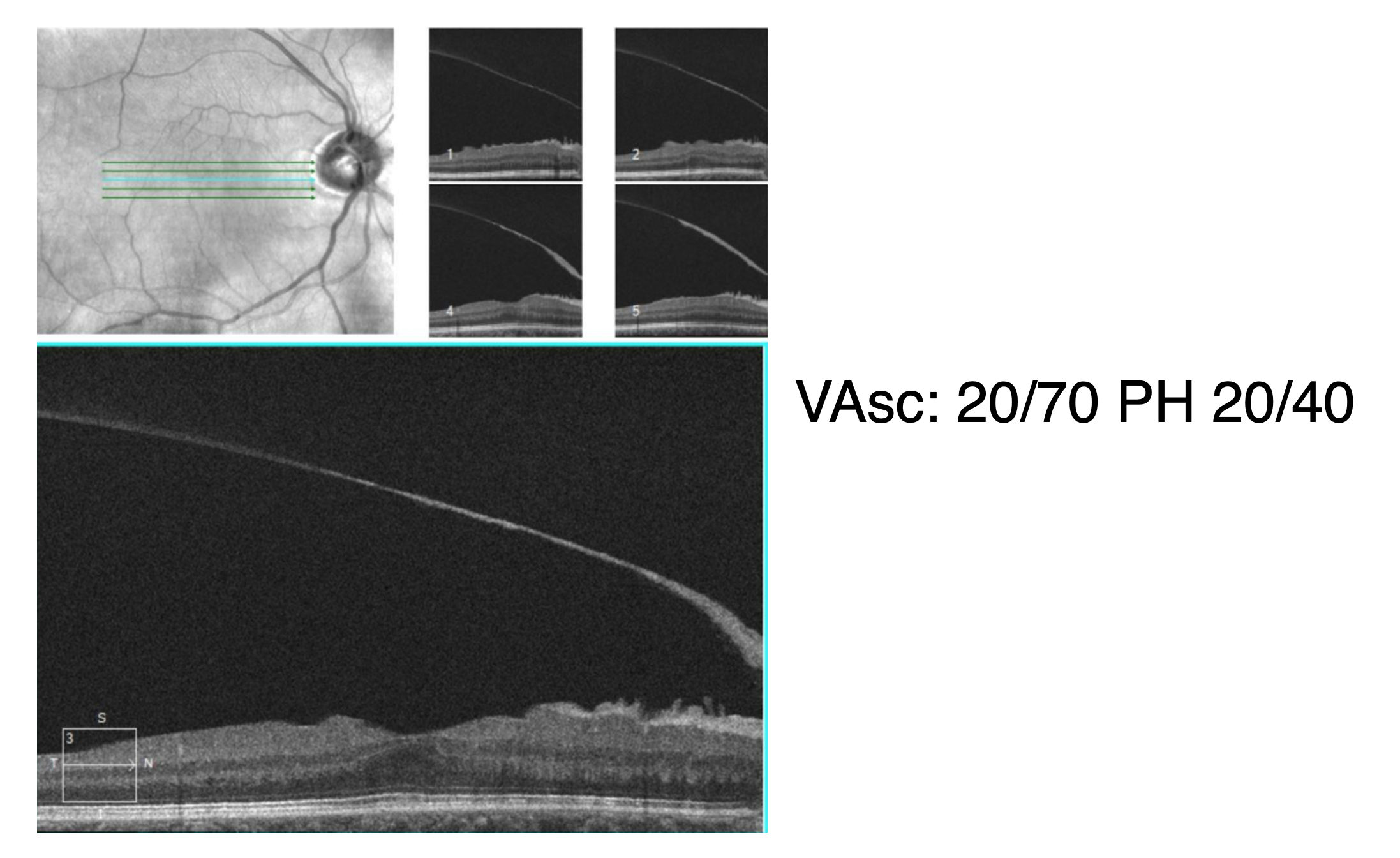
- 46 y.o. M presented with blurry vision OD for ~ 6-9 months
- PMH: shoulder surgery, vasectomy
- POH: none
- Systemic medications: none
- Ocular medications: none
Assessment
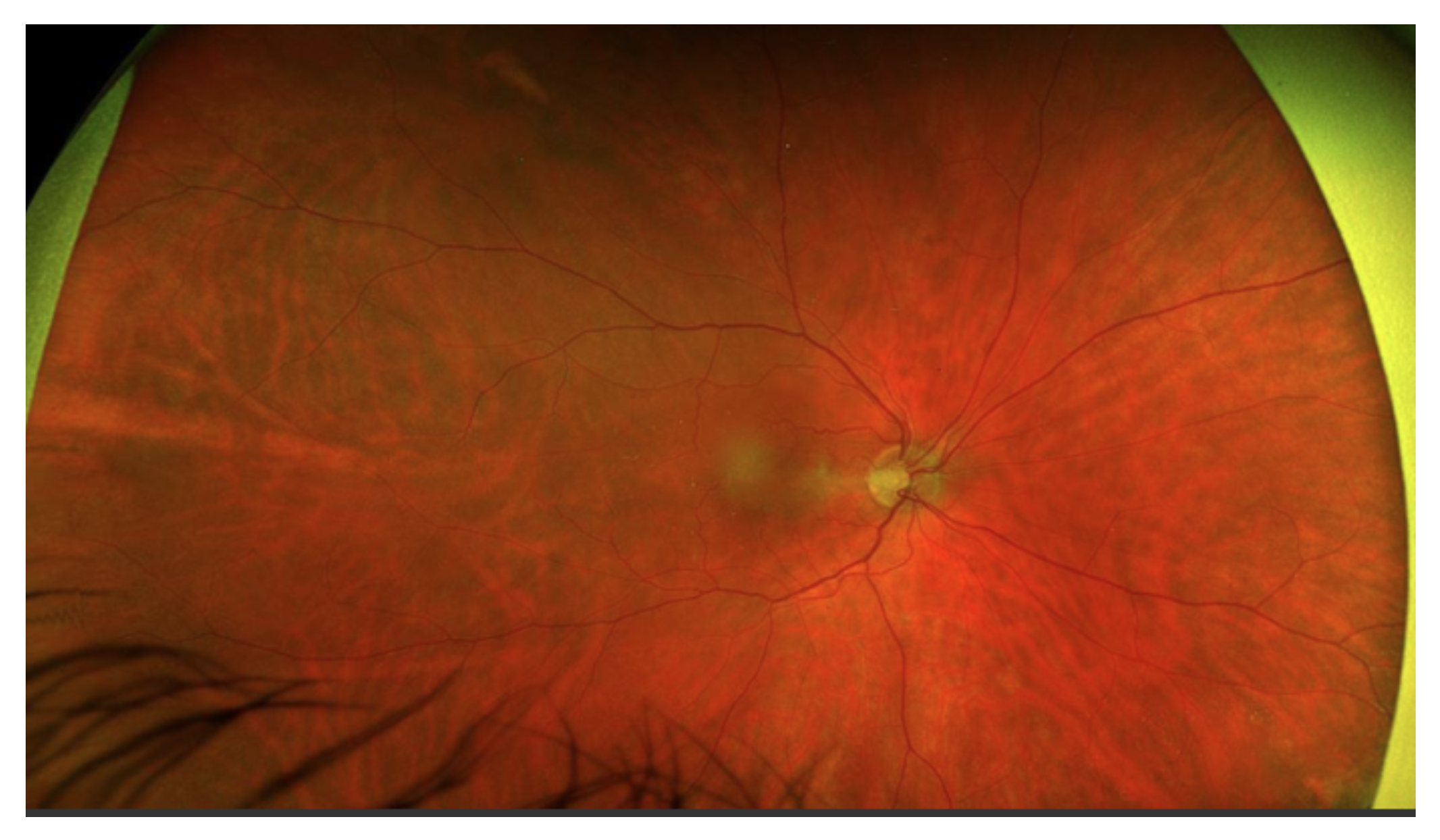
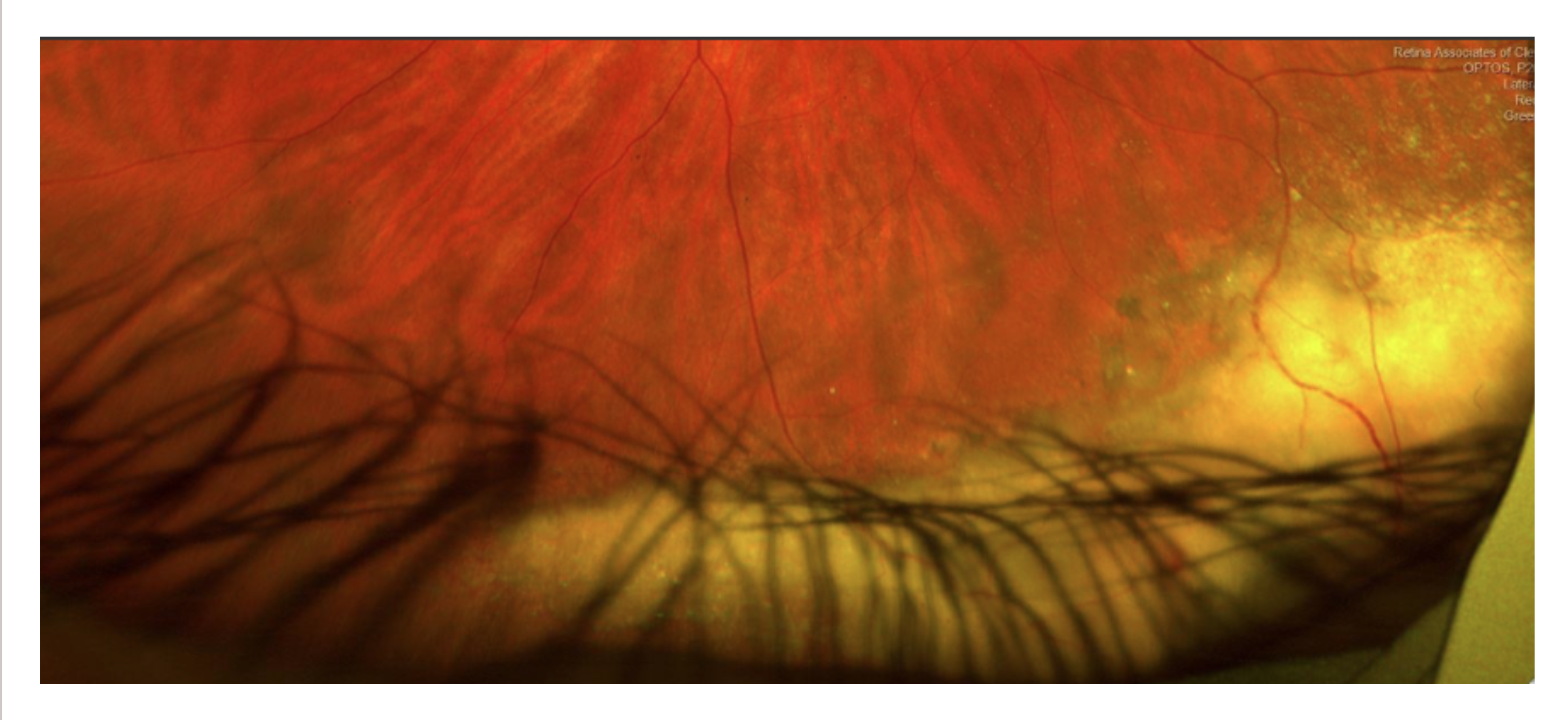
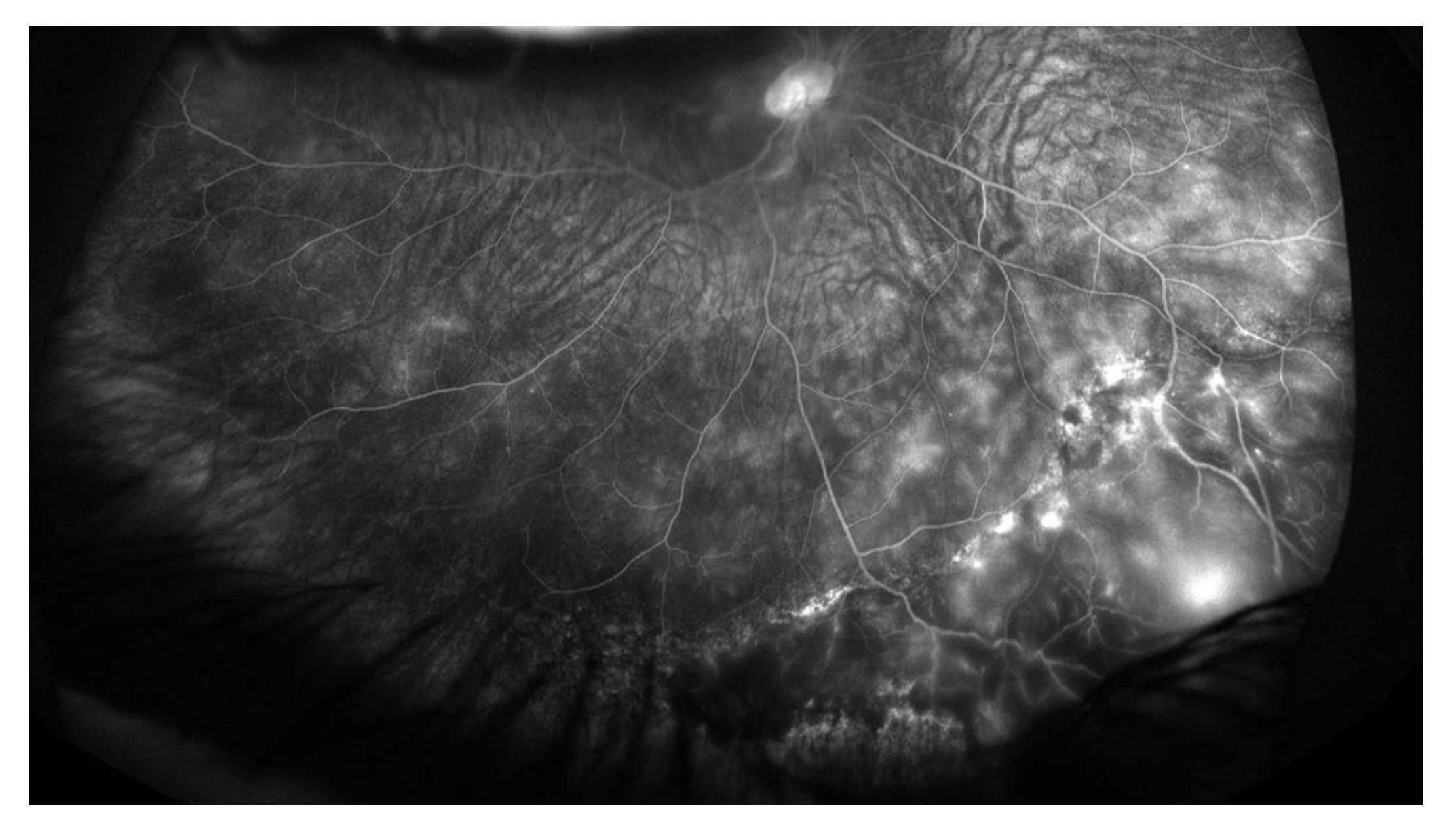
- This patient's exam is consistent with a PARG lesion (pseudoangiomatous retinal gliosis) in the setting of adult-onset Coats disease
- The ERM is secondary to these processes
Management
- Goal: stabilize the exudation/lesion medically prior to planning PPV with ERM peel
- Treated with sub-tenon's kenalog and anti-VEGF x2 for 2 months -> there was significant reduction of exudation
- After the injections, PRP applied to the areas of non-perfusion and laser was applied to the telangectatic vessels (vessels were “painted" with laser on low power and continuous duration) -> further reduction of exudation was noted and the PARG lesion essentially resolved
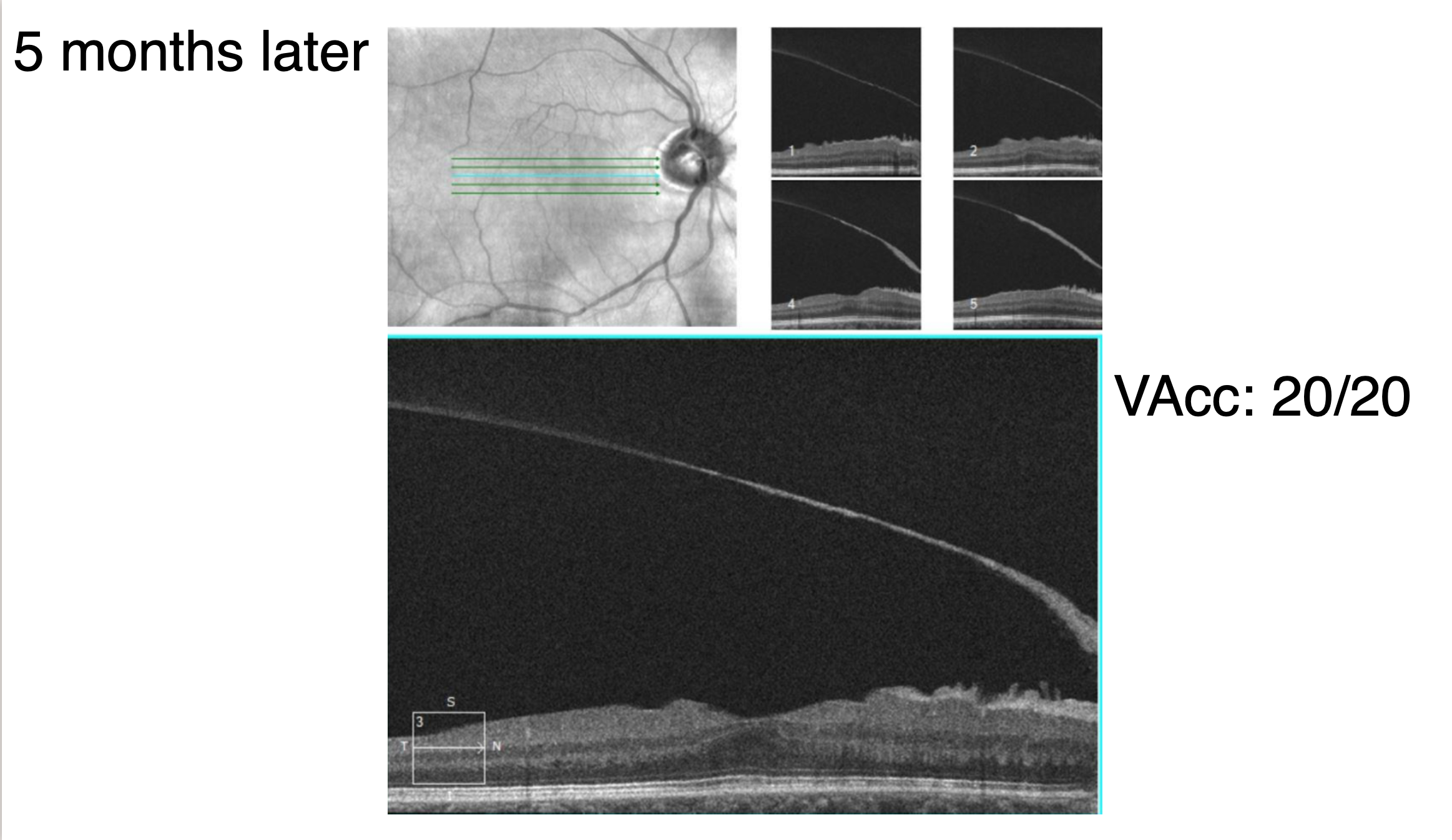
- Additionally, one month after the last PRP session the patient started to develop a PVD and the ERM self-peeled along with the hyaloid …...
Management
- At this point there, was no further exudation and as the membrane was self-peeling, no further intervention was undertaken
- The patient was monitored every 6-8 weeks with scleral depressed dilated exams and OCT
- No surgery has been needed
PARG
- Pseudoangiomatous retinal gliosis
- Also known as:
- Vasoproliferative retinal tumor (VPT)
- Presumed acquired retinal hemangioma
- Angioma-like retinal tumor
- Reactive retinal gliosis
- Reactive retinal astrocytic tumor
- Appearance:
- Gray-pink retinal mass
- Sub retinal lipid exudation
- Focal intralesional hemorrhages
- May have associated exudative retinal detachment
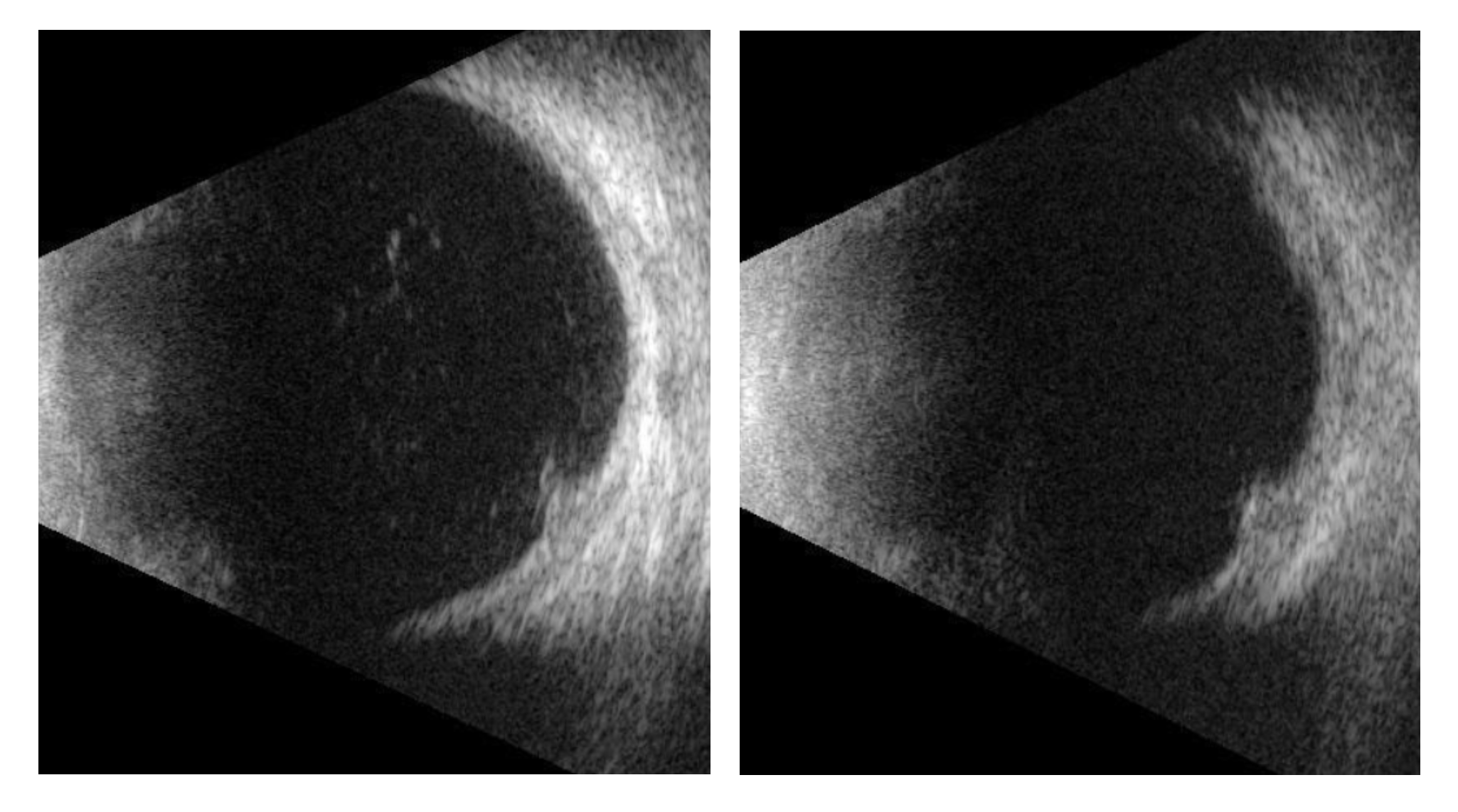
- B-scan:
- Medium to high internal reflectivity on A-scan
- Acoustic soliditiy without choroidal excavation
- Histophatology:
- Mostly glial cells, some vascular proliferation as well
- Can be a primary lesion (idiopathic) or secondary associated with underlying conditions such as:
- Retinitis pigmentosa
- Pars Planitis
- Coats disease
- History of retinal detachment surgery
- Retinal vasculitis
- FEVR
- Primary lesions are more common (74% of cases)
- Secondary VPT is more likely to be bilateral and associated with poorer visual acuity outcomes
- Commonly inferotemporal, mean age of presentation ~44 years
- Associated complications:
- Macular edema
- Macular exudation
- Sub retinal fluid, exudative retinal detachment
- Pre-retinal fibrosis
- Vitreous hemorrhage
- Differentiate from retinal capillary hemangioma (RCH)
- Not associated with Von Hippel-Lindau Syndrome
- No family history
- Lack of a feeder artery and draining vein
- Other lesions in the differential:
- Capillary hemangioblastoma
- PEHCR (peripheral exudative hemorrhagic chorioretinopathy)
- Choroidal melanoma
- RPE adenoma/adenocarcinoma
- Treatment
- Depends on size/location of lesion and whether it is causing vitreoretinal complications
- Modalities:
- Observation
- Laser
- Photodynamic therapy
- Plaque Radiotherapy
- Anti-VEGF injections
- Surgical excision (rare)
Self-peeling ERM
- Rare, 1-3% of all ERM cases
- Usually occurs in the process of an acute PVD where the connections between the ERM and the retina are severed
- Has also been reported following PRP and Nd:YAG poaterior capsulotomy
- When not occurring in association with acute PVD, it is thought that the contractile forces of the ERM are stronger than the ERM's connection to the retina and the ERM may self-peel
- Seen in younger patients where membranes tend to have more myofibroblast cells than those in older adults
- Has also been reported in the setting of Valsalva (heavy weight-lifting)
References:
Coulier J, Gribomont AC, De Potter P. Decollement spontane d'une membrane epimaculaire apres cryotherapie de tumeurs retiniennes vasoproliferatives: a propos d'un cas [Spontaneous peeling of the epimacular membrane after cryotherapy of retinal vasoproliferative tumors: report of a case]. Bull Soc Belge Ophtalmol. 2013;(322):49-54. French. PMID: 24923082.
Mansour AM, Mansour HA, Arevalo JF. Spontaneous release of epiretinal membrane in a young weight-lifting athlete by presumed central rupture and centrifugal pull. Clin Ophthalmol. 2014 Nov 13;8:2243-50. doi: 10.2147/OPTH.S74163. PMID: 25484573; PMCID: PMC4238755.
Marback EF, Guerra RL, Maia Junior Ode O, Marback RL. Retinal vasoproliferative tumor. Arq Bras Oftalmol. 2013 May-Jun;76(3):200-3. doi: 10.1590/s0004-27492013000300016. PMID: 23929086.
Marquez MA, Fortun J, Iyer P, Harbour JW, Haddock LJ. Pseudoangiomatous retinal gliosis (PARG) treated with iodine plaque in patient with chronic retinal detachment. Am J Ophthalmol Case Rep. 2022 Jun 11;27:101614. doi: 10.1016/j.ajoc.2022.101614. PMID: 35734079; PMCID: PMC9207220.
Menteş J, Nalçacı S. An Unusual Case: Self-separation of an Idiopathic Epiretinal Membrane. Turk J Ophthalmol. 2020 Mar 5;50(1):56-58. doi: 10.4274/tjo.galenos.2019.62372. PMID: 32167266; PMCID: PMC7086095.
Shields CL, Kaliki S, Al-Dahmash S, et al. Retinal Vasoproliferative Tumors: Comparative Clinical Features of Primary vs Secondary Tumors in 334 Cases. JAMA Ophthalmol. 2013;131(3):328–334. doi:10.1001/2013.jamaophthalmol.524