CASE OF THE MONTH: July 2023
Dislocated IOL


Disclosures: Alimera (consultant), Apellis (consultant), Bausch and Lomb (consultant), Eyepoint (consultant), Genentech (consultant, speaker’s bureau), Iveric Bio (speaker’s bureau), Regeneron (research), Regenxbio (research), Zeiss (research)
HPI
- Referring cataract surgeon reported that a patient was being sent in who had complicated cataract surgery and the IOL had fallen posteriorly.
- Patient is a 45 yo man
- History of RD OD s/p SB 1996 and OS s/p SB 2015
- Recent cataract surgery right eye 2 weeks prior
- Current glasses: OD -4.25D, OS -9.25D
- Currently on the following drops OD:
- PF q2 hours
- Ofloxacin TID
- Cosopt BID
- Latanoprost qhs
- Cyclopentolate BID
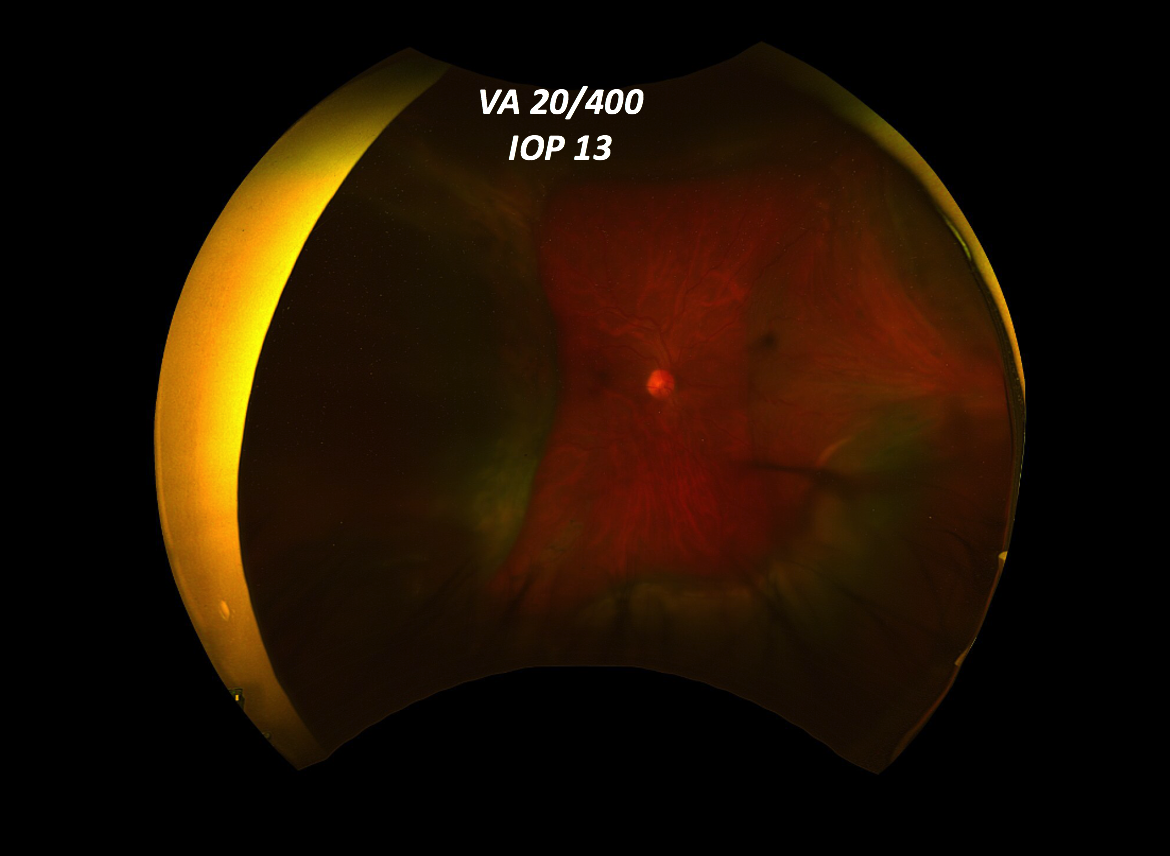
Retinal exam revealed elevation of the retina concerning for hemorrhagic choroidals but it was difficult to rule out a superimposed retinal detachment.
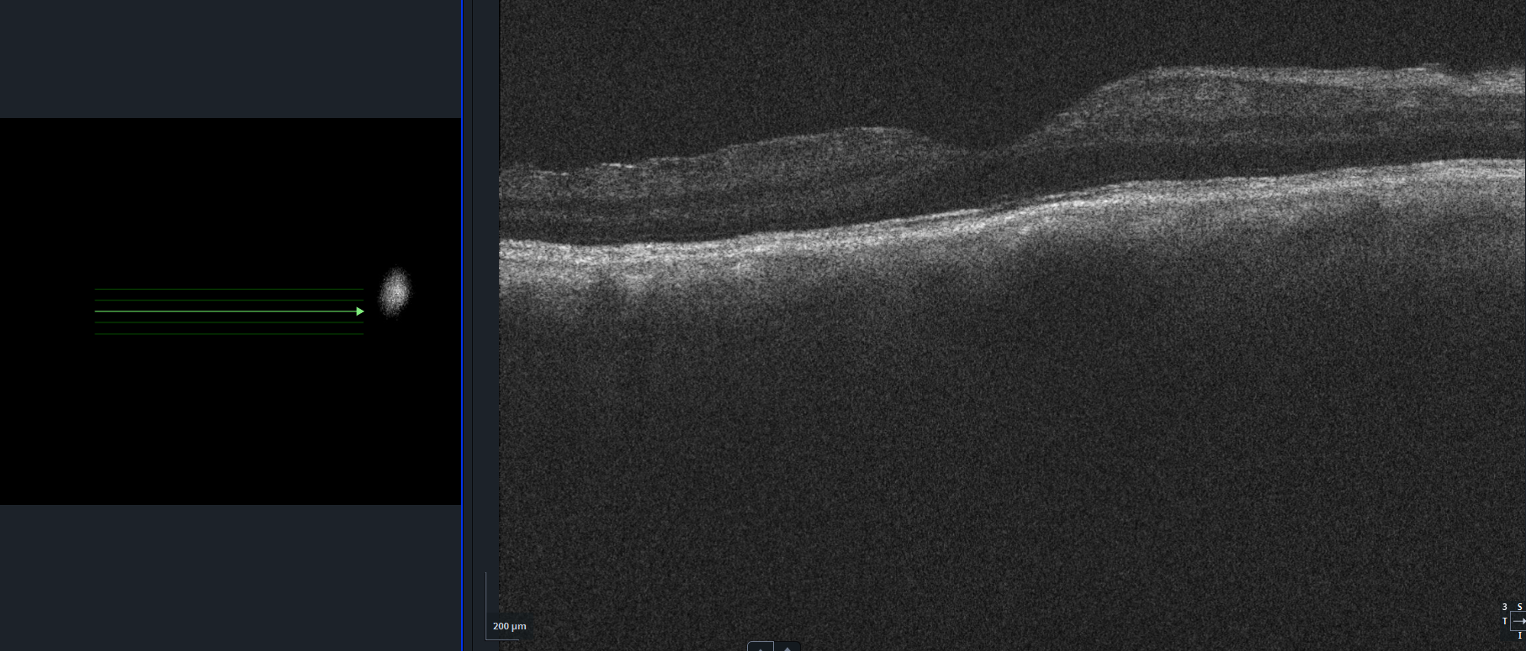
OCT revealed an attached macula
Where is the IOL?
The referring cataract surgeon had reported that the IOL had fallen to the back of on the eye but it is not seen on the fundus photos.
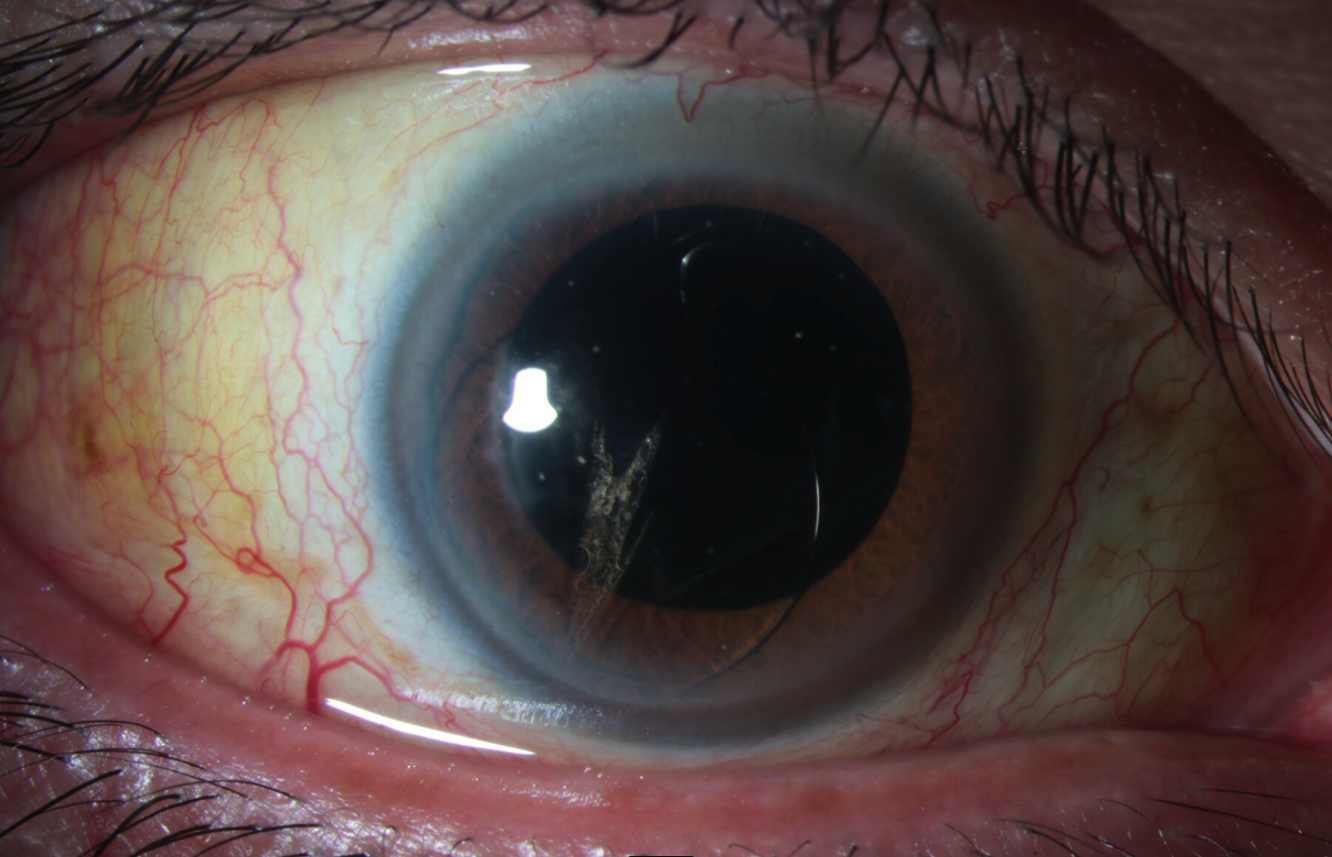
Anterior exam revealed a one-piece IOL in the anterior chamber. It appears the lens was attempted to be cut. One of the haptics was not visualized.
Other tests?
B scan
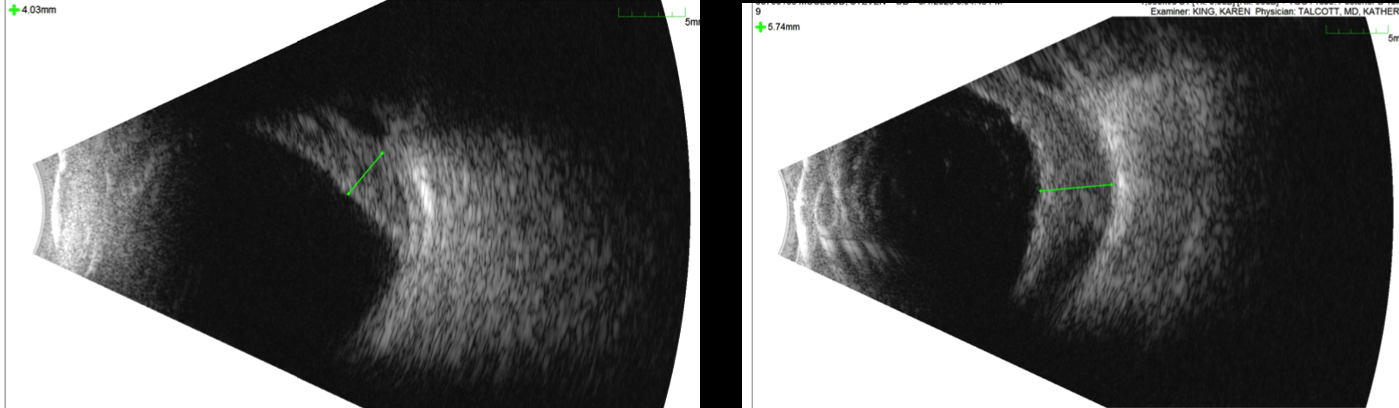
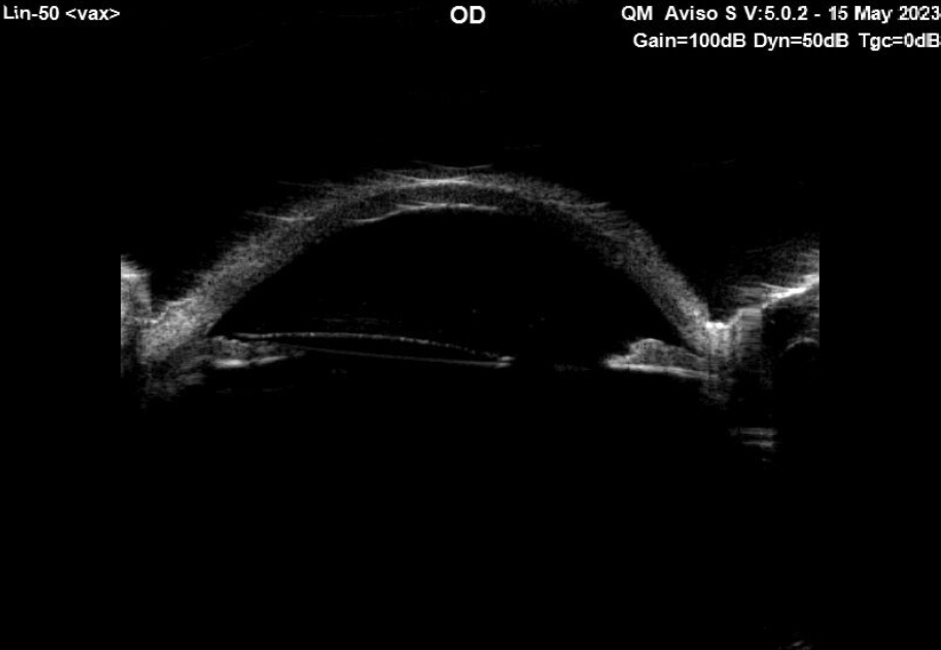
The B scan confirmed the presence of hemorrhagic choroidals with a maximum height of 5.7mm. No retinal detachment was seen.
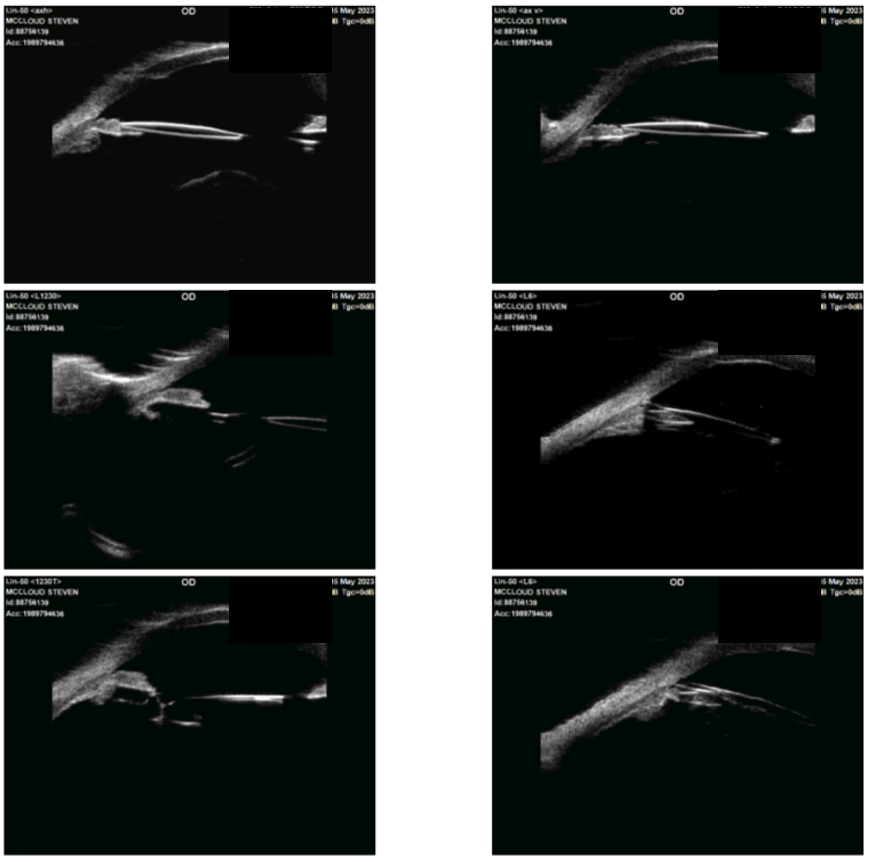
A UBM was also performed. The ultrasonographers reported that the IOL appeared to go through the iris and the “missing” haptic was posterior to the iris.
Management
- Where is the haptic?
- What kind of lens is this?
- When would take them to the OR?
- What would your surgical plan be?
- What do you tell the patient?
Patient Course
- Added oral prednisone, tapered IOP lowering drops
- Waiting for hemorrhagic choroidals to improve
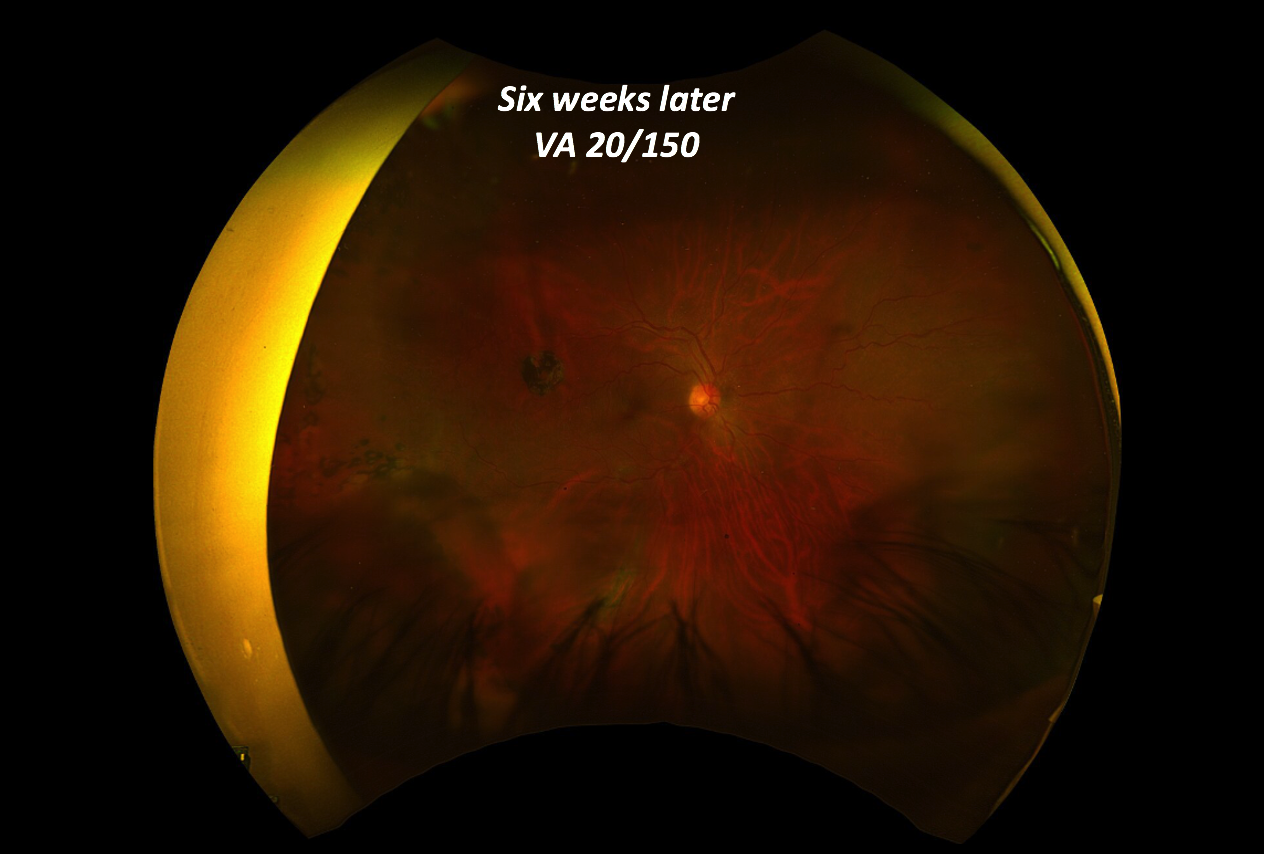
Retinal exam revealed significant improvement in the hemorrhagic choroidals
Repeat B scan
B scan also revealed improvement in the height of the hemorrhagic choroidals.
Surgical Repair
The patient underwent surgical repair. There was some concern that the IOL could be a PMMA lens given the prior attempt to cut it. Intraoperative examination revealed the ”missing” haptic was no longer attached to the IOL, which appeared to be acrylic. The decision was then made to proceed with an IOL exchange with an Envista MX60 lens in light of the patient’s prior retinal detachment. This exchange was performed through a clear corneal wound rather than a scleral tunnel, which would have been preferred for a larger wound required if the lens had been a PMMA lens.