CASE OF THE MONTH: January 2022
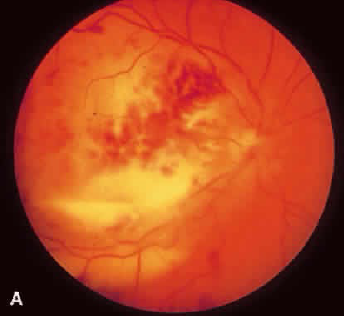
White stuff in the retina

History:
- HPI: 30 y/o woman s/p failed kidney transplant admitted for spiking a fever during dialysis session
- Past Ocular History: None
- Past Medical History: Nephrotic syndrome s/p kidney transplant x 2 (both failed)
- Multiple prior infections including pseudomonas peritonitis and pneumonia
- Currently immunosuppressed with tacrolimus and prednisone
- Current anti-infectious agents include:
- Active infection: Cefepime, Metronidazole
- Prophylaxis: Bactrim, Valganciclovir
- Sent to ICU and treated for sepsis
- Reason for ophthalmology consultation: "Look for fungal or other manifestations of infection in the eye"
- Patient has altered mental status but denies ocular complaints
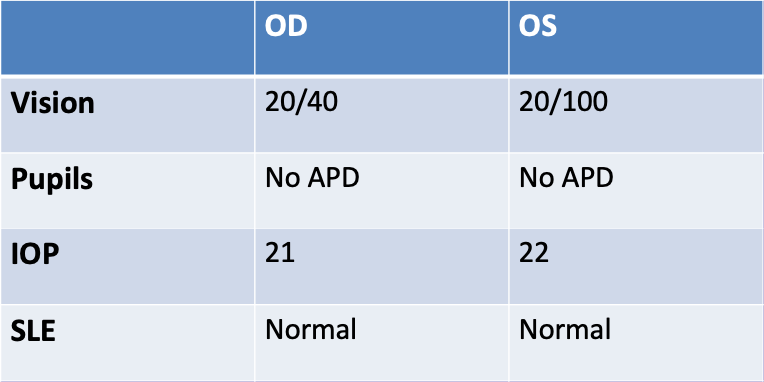
Exam
The case:
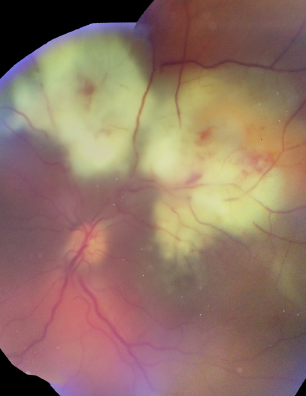
Differential Diagnosis: "white stuff" in the retina
- Viral retinitis
- CMV
- HSV
- VZV
- Fungal
- Bacterial
- Ischemia
- Inflammatory
Assessment and Plan
- Intravitreal injection of foscarnet OS for presumed CMV retinitis
- Anterior chamber paracentesis
- PCR for HSV, VZV, CMV
- Start IV ganciclovir
Clinical Course
- Blood negative for CMV
- Aqueous negative for CMV, HSV, VZV
- Repeat exam 5 days post foscarnet injection reveals new exudative RD and subretinal hypopyon
New Diagnosis – Aspergillus Retinitis
The case for Aspergillus Retinitis
- Sputum fungal culture + for Aspergillus
- Respiratory culture + for Aspergillus
- Fungitell (β-D-Glucan): 35,120 (off the charts)
- Blood cultures negative during this hospitalization
- CT chest and MR brain have lesions consistent with infectious process
- Intravitreal voriconazole injection OS
- IV voriconazole
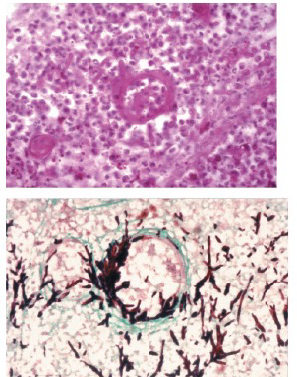
Aspergillus retinitis
Epidemiology
- 2nd most common cause of fungal endophthalmitis after candida
- Risk factors:
- IV drug abuse
- Immune deficiency (organ transplant patients)
- Corticosteroid use
- Pathogenesis
- Hematogenous spread of infection to choroid
- Proliferation of fungus in blood vessels promotes ischemia and necrosis
Riddell J et al. Medicine. 2002.
Rao N et al. Am J Ophthalmol. 2001
Clinical Manifestations
Weishaar PD et al. Ophthalmology. 1998
Making the diagnosis of aspergillus retinitis
- Blood cultures and aqueous/vitreous cultures often negative for aspergillus
- Appropriate clinical context
- Immunosuppressed
- Aspergillus elsewhere
Bodoia R et al. Retina. 1989
Treatment
- No RCTs to guide choice/duration of therapy
- Systemic therapy with:
- Amphotericin B or Voriconazole
- Intravitreal therapy with:
- Amphotericin B or Voriconazole
Prognosis
- 8% of patients regained useful vision in one series (endophthalmitis + retinitis)
- Poor initial vision predicts poor outcome
- 50% mortality
Riddell J et al. Medicine. 2002.
Clinical Course
- Most recent repeat exam 12 days post intravitreal voriconazole shows improvement with resolved exudative detachment and smaller area of retinal whitening.
- Was doing well systemically and transferred from ICU to floor
- One day after the most recent eye exam, she developed acute mental status change and aphasia
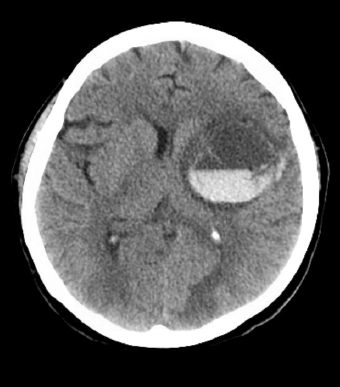
- Transferred back to ICU
- Underwent hemicraniectomy with partial clot evacuation
- Neurologic status worsens with decerebrate posturing
- Decision made to make her comfort measures and she passes away
Key Points
- Retinal whitening in an immune compromised patient should raise concern for HSV/VZV/CMV
- Aspergillus retinitis can look like CMV
- Talk to Infectious Diseases and review systemic labs/imaging for help making diagnosis
Acknowledgements
Tatiana Deveney, MD
Devon Ghodasra, MD
Daniel Kaul, MD
Joseph Grubbs, MD
Tyson Kim, MD, PhD
Vaidehi Dedania, MD
Meti Munie, MD
Lev Prasov, MD, PhD
Jonathan Trobe, MD