CASE OF THE MONTH: January 2023
I'm doing just fine


Case Presentation
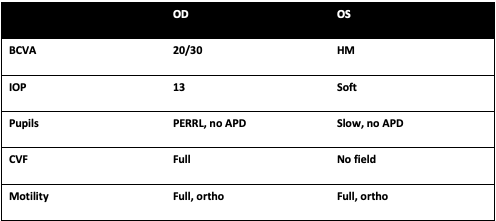
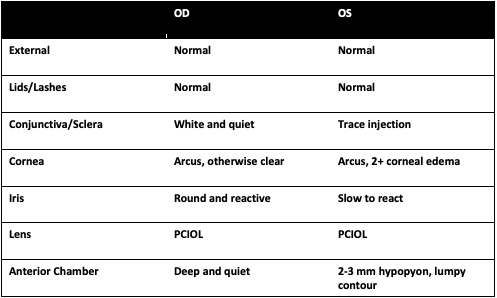
A 76 year-old male presents with a month long history of worsening vision in the left eye. His retina specialist referred him for recalcitrant uveitis with a concern for intraocular lymphoma give his lack of improvement on oral steroids.
History
PMHx: Diabetes, COPD, multiple myeloma, cardiac ablation, stage 3 chronic kidney disease, pleural effusions
- POHx: Cataract surgery both eyes, vitrectomy left eye
- SHx: Lives with this wife, no other significant history
- FHx: none
- Allergies: none
- Rx: none
- ROS: No recent fevers, chills, sick contacts, or neurological changes
Exam
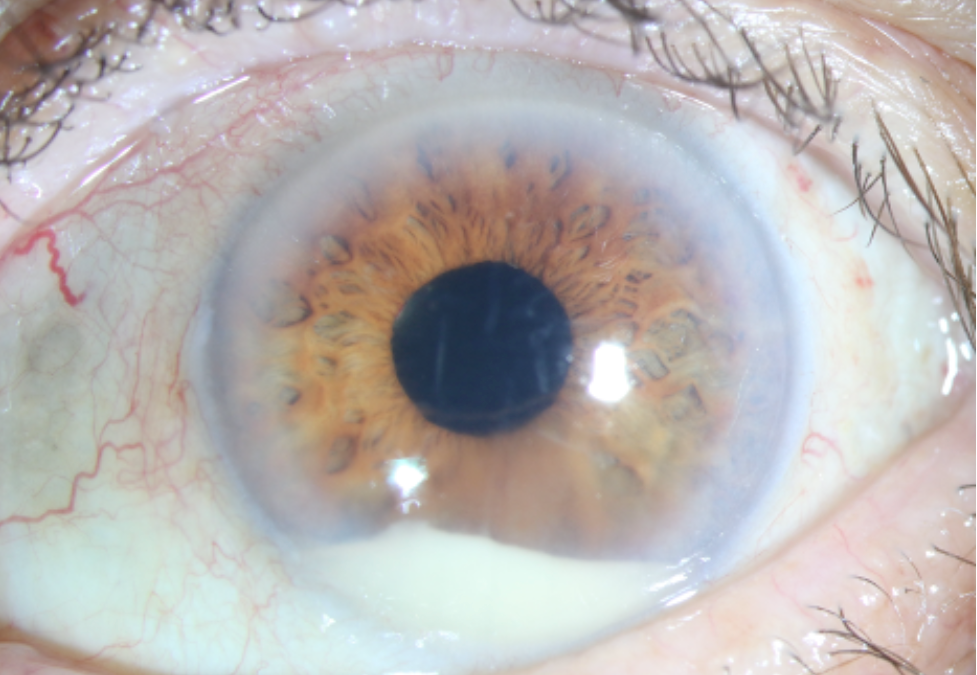
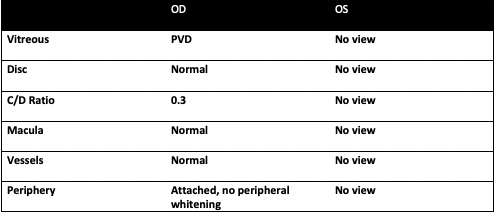
Slit lamp photograph displaying a hypopyon with a lumpy contour. Strikingly, the conjunctiva has very little injection, which is unexpected given the marked anterior chamber reaction. This mild of an appearance is atypical for endophthalmitis; however, we his oral steroids were likely masking the full range of his symptoms.
Summary of Findings
- A 76-year-old male presented from an outside provider for worsening vision over the last month. He had been followed for anterior and intermediate uveitis (described as a small hypopyon and vitreous cell), but his inflammation worsened on topical therapy. Given his lack of improvement with topical steroids, there was a concern for lymphoma and he underwent a diagnostic vitrectomy with this outside specialist. At the same time, vitreous samples were sent for bacterial, fungal and viral evaluation.
- Per the outside provider, there was no retinal whitening, signs of infection, or vasculitis noted intraoperatively and the vitreous samples revealed no infectious growth or signs concerning for lymphoma on pathology. The patient was then started on oral prednisone (60 mg) for two weeks before being sent to our center given the persistent hypopyon but minimal pain or injection. The patient’s main concern at this visit was his blurred vision.
- Anterior examination: The right eye was white and quiet with no signs of anterior or posterior inflammation. The left eye had trace injection, trace pain with palpation, a 2 to 3 mm hypopyon with a lumpy surface and no view posteriorly.
- Posterior examination: The right eye was normal with no signs of posterior whitening or lesions; the left eye had no view. B scan showed dense vitreous debris and concern for a shallow retinal detachment.
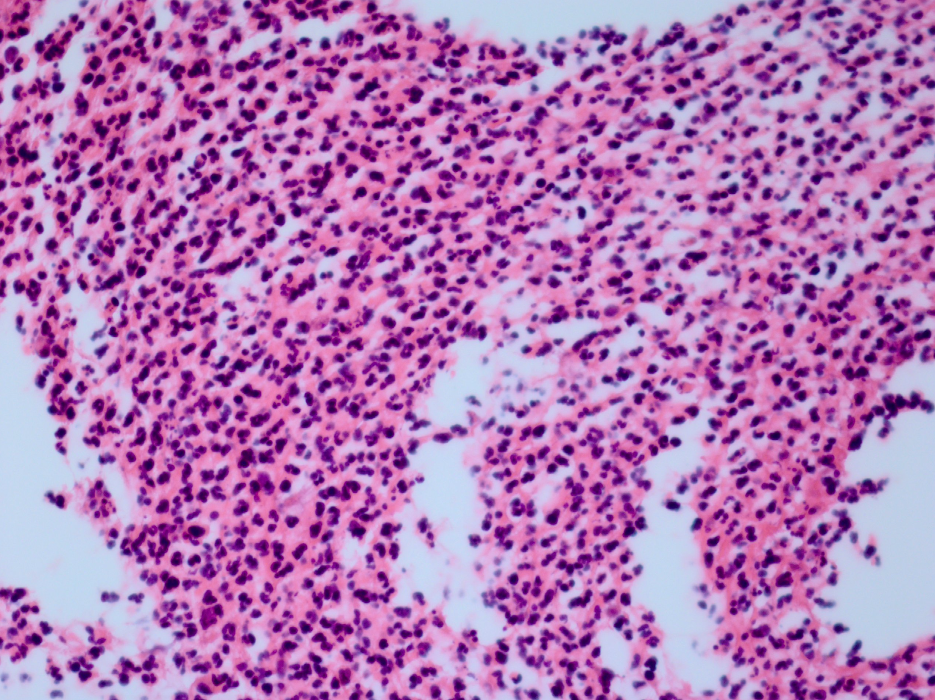
- On presentation to Emory he underwent an anterior chamber tap given the concern for infection. The preliminary gram stain showed no growth, but did have rare polymorphonuclear leukocytes. Given atypical presentation of very little pain and injection despite a hypopyon, his slides were also reviewed by our pathologist who confirmed signs of inflammation with a large number of neutrophils.
Mechanism and differential diagnosis (Endogenous endophthalmitis)
- Endogenous endophthalmitis, a potentially blinding intraocular infection arises from the hematogenous spread of a primary source. This source is often bacterial or fungal.
- Endogenous endophthalmitis accounts for a small percentage of cases of endophthalmitis overall (2-8%).1
- Patients with a history of immunocompromise or hypogammaglobulinemia, such as this patient with multiple myeloma, are at increased risk of endogenous endophthalmitis. 1 Additionally, patients with a history of invasive procedures or intravenous drug use are at risk of developing the disease.
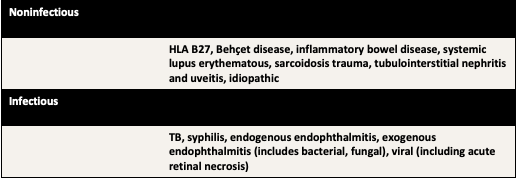
- Patients usually present with a constellation of symptoms similar to panuveitis or a combination of anterior and intermediate uveitis. The differential for either are summarized in the below table [1]
- In patients treated with steroids, the signs of endophthalmitis can become masked, as with our patient, who presented with very little injection or pain.
Workup
Broad uveitis and infectious workup sent:
- Blood cultures, urine culture, chest x ray, CBC, CMP, ACE, HLA-B27, RPR, syphilis IgM/IgG, Quant-gold, Toxoplasmosis IgM/IgG
- AC Tap sent for viral (CMV, VZV, HZV) and toxoplasmosis PCR, gram culture and stain, fungal culture, and pathology review
- Gram stain and culture: multiple polymorphonuclear leukocytes, no bacterial or fungal organisms seen.
- Pathology review: Multiple neutrophils seen
Treatment & clinical course
- Although there were no organisms seen on ocular culture, the presence of neutrophils was concerning for an infection. The patient was given intravitreal vancomycin and ceftazadime for presumed infection and advised that his retinal detachment would be addressed after he was worked up for sepsis.
- He was admitted to the hospital near his home for a sepsis work up– blood cultures and urine cultures were drawn but the results are unavailable. His vitals were significant for low blood pressure and tachycardia. Chest X ray showed bilateral pneumonia and he was admitted for intravenous antibiotics. At this point it was presumed that his endogenous endophthalmitis had seeded from his pneumonia. Unfortunately, he passed away shortly after admission from sepsis related complications and cardiac instability.
Discussion
- Endogenous endophthalmitis presents a diagnostic and therapeutic challenge to clinicians, and can result in irreversible vision or globe loss, along with systemic complications. 2
- Additionally, the source of the infection must be controlled. In cases of suspected endogenous endophthalmitis, a work up for infectious sources should be initiated immediately, including blood and urine cultures, and in certain cases, chest and cardiac imaging (especially in the case of prior cardiac surgery/implants).
- Endogenous endophthalmitis can result from various pathogens after hematogenous spread, with the most common gram-positive organisms being Staphylococcus and Streptococcus, and the most frequent gram-negative organisms being Pseudomonas.3
- Patients who are immunocompromised, have a history of intravenous drug use, or have undergone invasive procedures are at risk. In our patient, his multiple myeloma and resultant hypogammaglobulinemia placed him at higher risk for developing endogenous endophthalmitis.1
- Steroids can mask the appearance and symptoms of endophthalmitis; despite having less injection and pain, the steroid will eventually lead to the worsening of infection without appropriate treatment aimed at the infection.4 In our case, the patient's presentation was milder than expected for endogenous endophthalmitis that had been brewing for several weeks, likely secondary to the oral steroids he was placed on.
- In cases where the presumed inflammation does not improve on oral steroids, it is always important to consider the possibility of infection.
1. Romero CF, Rai MK, Lowder CY, Adal KA. Endogenous endophthalmitis: case report and brief review. American family physician. 1999;60(2):510-514.
2. Chee SP, Jap A. Endogenous endophthalmitis. Current opinion in ophthalmology. 2001;12(6):464-470.
3. Danielescu C, Anton N, Stanca HT, Munteanu M. Endogenous Endophthalmitis: A Review of Case Series Published between 2011 and 2020. Journal of ophthalmology. 2020;2020:8869590.
4. Fung AT, Tran T, Lim LL, et al. Local delivery of corticosteroids in clinical ophthalmology: A review. Clinical & experimental ophthalmology. 2020;48(3):366-401.