CASE OF THE MONTH: December 2022
It's Just Floaters


Case Presentation
71-year-old male presents with 1 week history of new floaters in the left eye. Denies eye pain and photophobia. Denies trauma. Patient was evaluated 3 days prior and diagnosed with an evolving posterior vitreous detachment.
History:
- POHx: none
- PMH: Genital herpes simplex virus (last flare 1 month ago, not on prophylactic medication), Hyperlipidemia
- Medication: None
- SHx: Denies illicit drug house. Denies risky sexual behavior. Former smoker (1 pack per day). Previously owned a cat.
- FHx: Mother with glaucoma.
- Allergies: none
- Rx: none
- ROS: (-) fevers, chills, nausea, vomiting, diarrhea, shortness of breath, cough, or dyspnea.
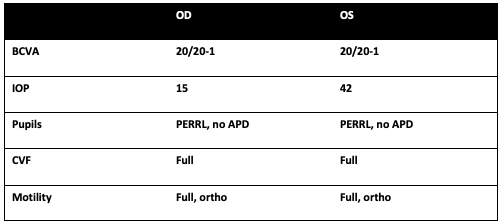
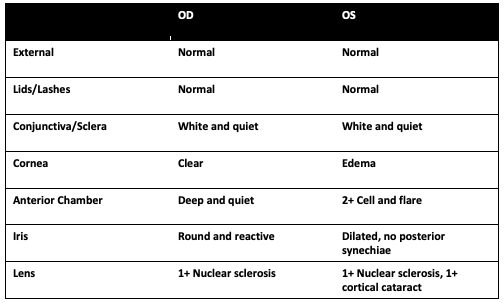
Exam
Summary of Findings
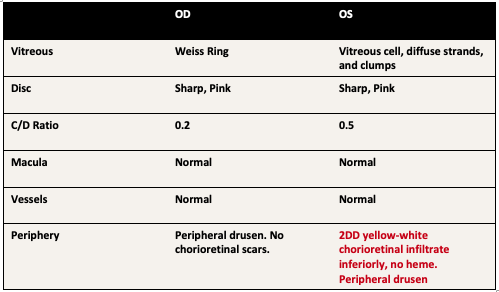
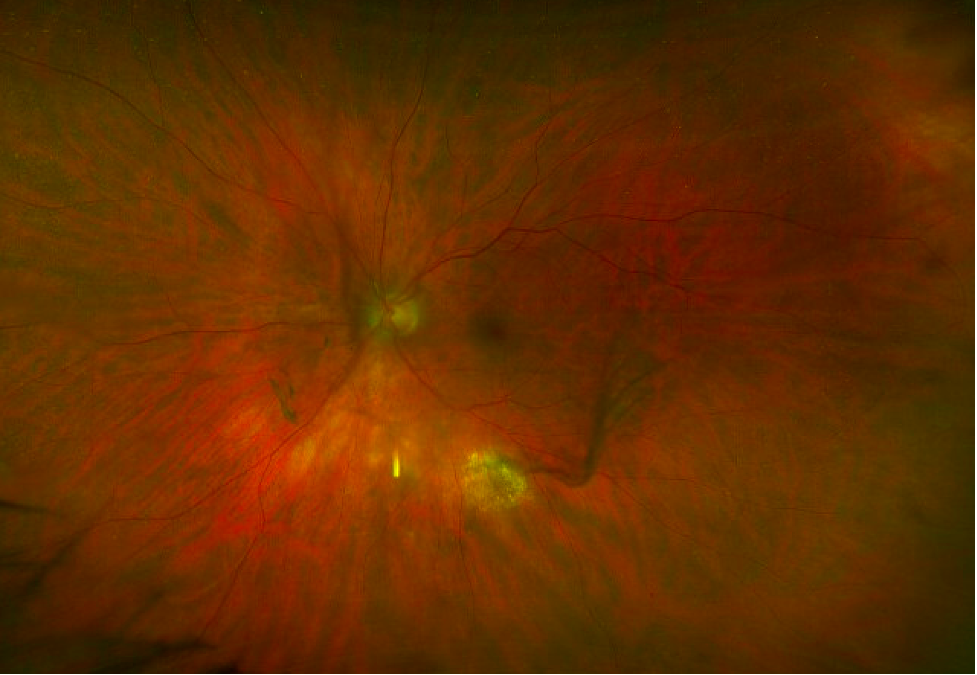
- 71 year-old male presents with 1 week of floaters his left eye. He was found to have elevated intraocular pressure and panuveitis with vitreous strands and clumping and a single extramacular chorioretinal infiltrate inferiorly in the left eye.
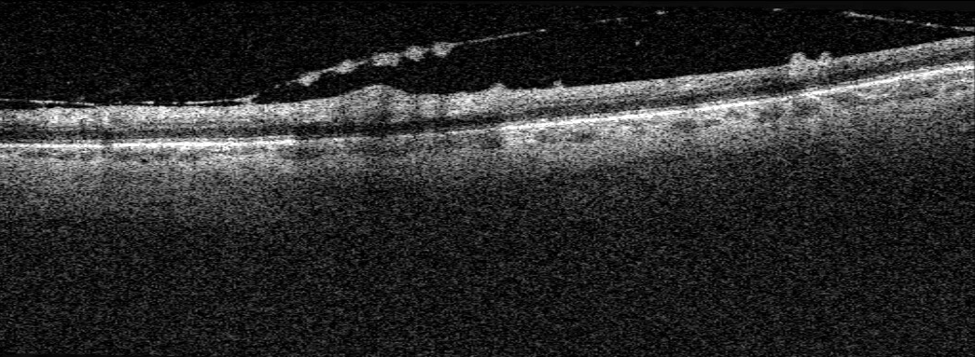
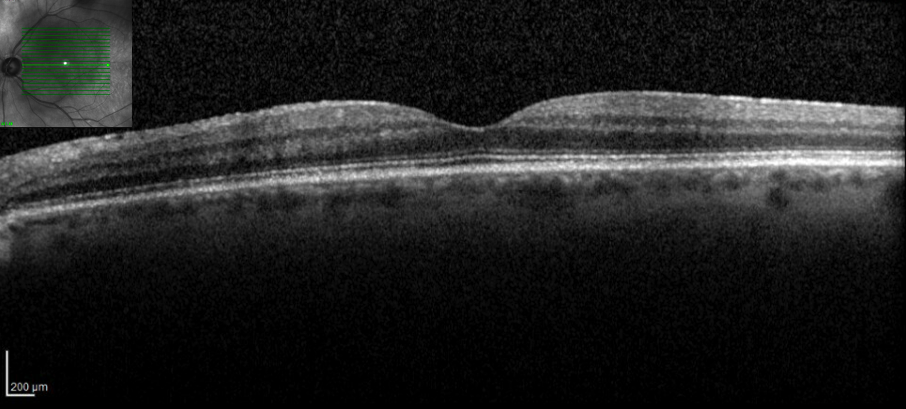
- OCT: Thickening of the posterior hyaloid with hyperreflective deposits along the posterior hyaloid face and vitreoretinal interface. Full thickness hyperreflective retinal lesion inferior to macula.
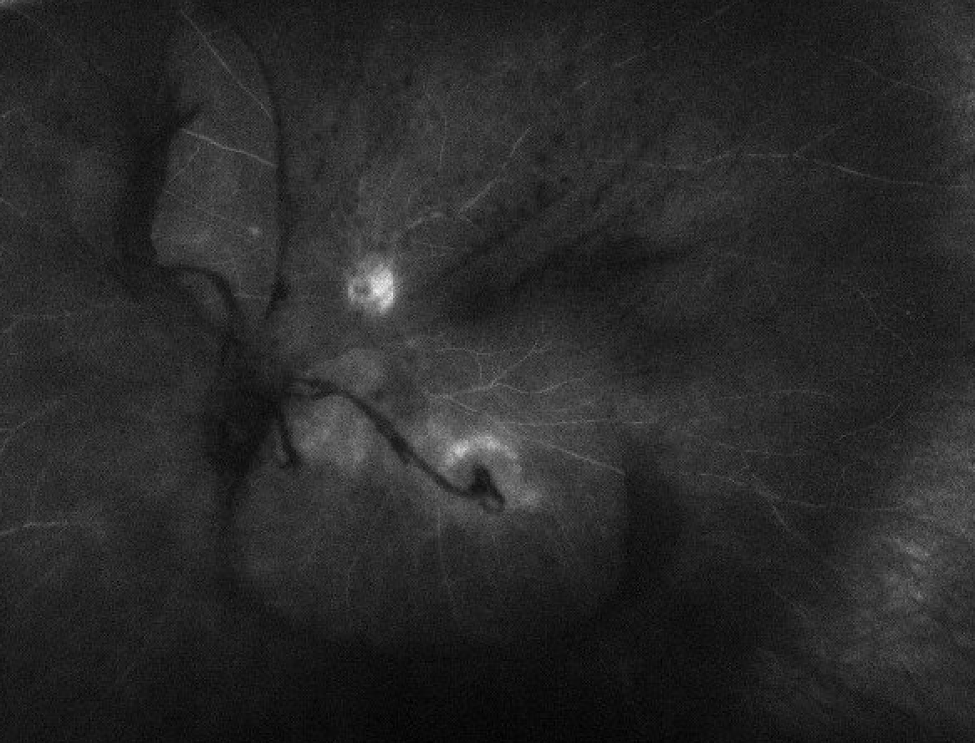
- FA: Staining surrounding inferior lesion, late disc staining. Mild, diffuse vascular leakage.
Differential diagnosis
- Inflammatory
- Behcet's Disease
- Sarcoidosis
- White Dot Syndromes (Multifocal choroiditis with panuveitis)
- Idiopathic Panuveitis
- Infectious
- Syphilis
- Tuberculosis
- Primary Toxoplasmosis gondii
- Viral retinitis
- Acute Retinal Necrosis
- CMV Retinitis
- Endogenous bacterial endophthalmitis
- Endogenous fungal endophthalmitis
- Toxocariasis
- Malignancy
- Primary Vitreoretinal Lymphoma
- Metastasis
Workup
Normal results:
- CBC, CMP, Blood cultures
- ACE, Lysozyme, RF, Anti-CCP
- RPR, FT-Abs, Quantiferon-gold, HIV
- Anterior chamber tap for viral PCR
- Vitreous tap for toxoplasmosis PCR and fungal cultures
Significant findings:
- Serum Toxoplasmosis IgG elevated, IgM normal
Treatment & clinical course
- At presentation, the patient received injection of intravitreal Foscarnet (2.4mg/0.1ml) and was started on Valtrex 1 gram three times a day for acute retinal necrosis given recent HSV1 flare
- Once the aqueous PCR results returned negative for HSV/VZV/CMV, the Valtrex was stopped and the patient was started on Bactrim DS tablets twice per day for 6 weeks to cover for Toxoplasmosis
- Oral prednisone 60 mg daily with a 6-week taper course was initiated after syphilis screening (RPR/FT-Abs) and tuberculosis screening (Quantiferon Gold) returned negative
- Drop regimen included prednisolone every hour, cyclopentolate twice per day, and brimonidine/timolol twice per day (for increased intraocular pressure)
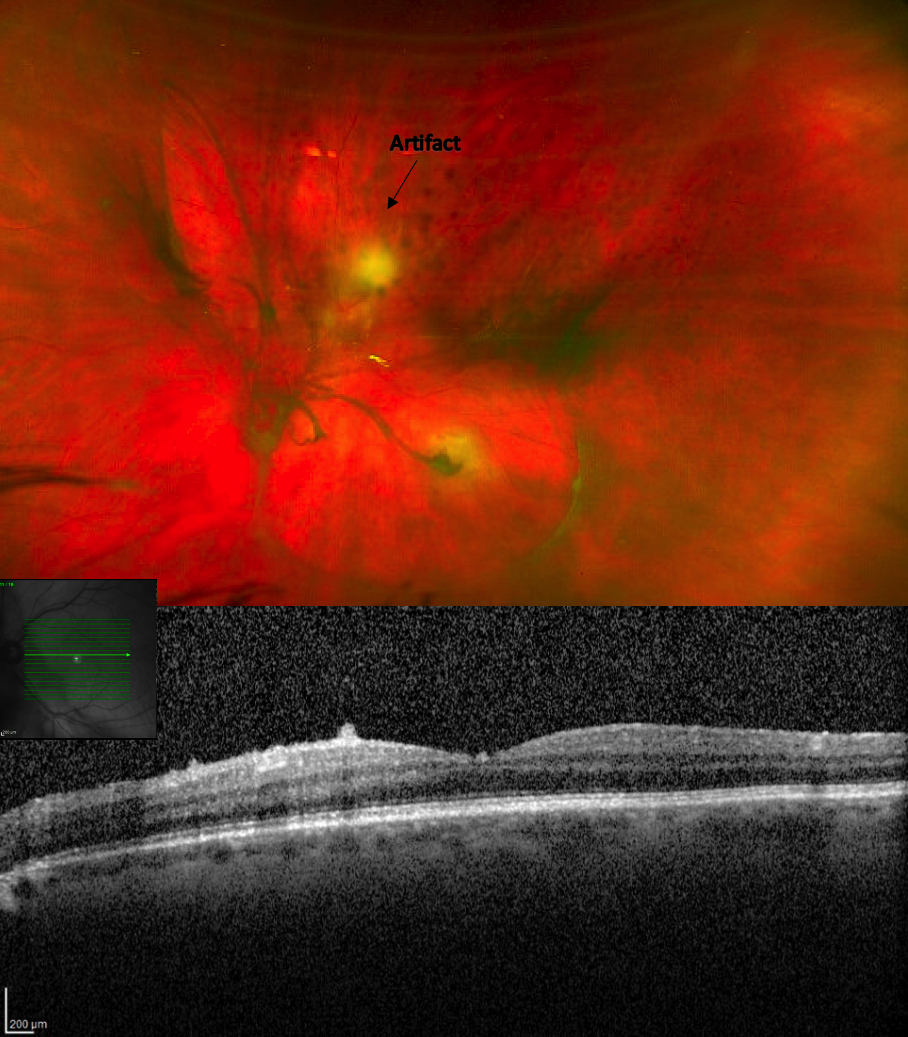
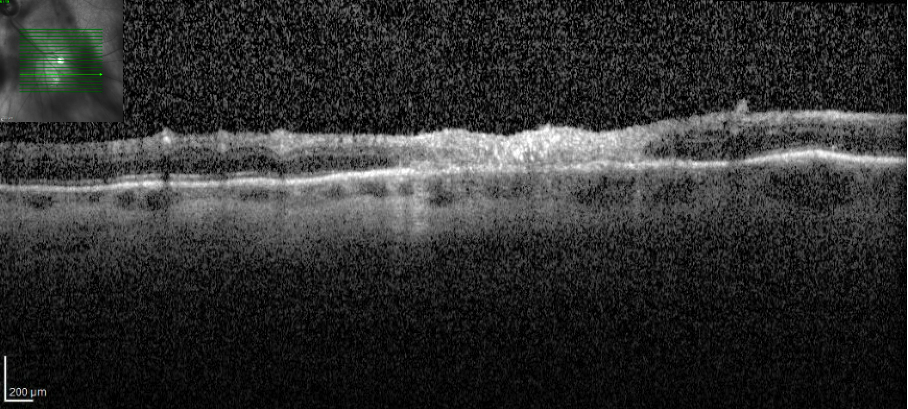
OCT 6 weeks after presentation demonstrating a trace epiretinal membrane and resolution of hyperreflective deposits along the vitreoretinal interface
Discussion
- This 71 year old healthy male was diagnosed with primary ocular toxoplasmosis (OT)
- OT is the most common cause of infectious chorioretinitis globally1
- While OT can occurs in immunocompetent individuals, a thorough history and select work-up should be performed to ensure no risk factors for an immunocompromised state are present
- In immunocompetent individuals, aqueous sample PCR for toxoplasmosis is only positive in 30-40% of clinically diagnosed cases and vitreous sample PCR is only positive in up to 50% of cases2. In addition, while a negative serum Toxoplasmosis IgG can help rule out OT in an immunocompetent patient, a positive IgG alone is not conclusive, given the high prevalence of toxoplasmosis2. As such, clinical exam and in-office testing are essential in making the diagnosis
- OCT findings of full thickness hyperreflective retinal lesion are highly suggestive of OT3. Thickening of the posterior hyaloid and hyperreflective deposits along the posterior hyaloid face and vitreoretinal interface can also be found with OT3,4 and this presentation is highly suspicious for OT
- Other vision threatening infectious etiologies should be ruled out including acute retinal necrosis, bacterial endophthalmitis, fungal endophthalmitis, syphilis, and tuberculosis.
- Various treatment modalities exist including systemic pyrimethamine, sulfadiazine, and corticosteroids, systemic trimethoprim/sulfamethoxazole, systemic azithromycin, and intravitreal clindamycin5
1. Holland, G. N., Lewis, K. G. & O'Connor, G. R. Ocular Toxoplasmosis: A 50th Anniversary Tribute to the Contributions of Helenor Campbell Wilder Foerster. Archives of Ophthalmology 120, 1081–1084 (2002).
2. Garweg, J. G., de Groot-Mijnes, J. D. F. & Montoya, J. G. Diagnostic Approach to Ocular Toxoplasmosis. Ocular Immunology and Inflammation 19, 255–261 (2011).
3. Guagnini, A.-P., Potter, P., Levecq, L. & Kozyreff, A. Atypical spherical deposition on vitreoretinal interface associated with toxoplasmic chorioretinitis. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv für klinische und experimentelle Ophthalmologie 245, 158–60 (2007).
4. Adıyeke, S. K. et al. Optical coherence tomography findings in toxoplasma retinochoroiditis. Indian Journal of Ophthalmology , (2021).
5. Ozgonul, C. & Besirli, C. G. Recent Developments in the Diagnosis and Treatment of Ocular Toxoplasmosis. Ophthalmic Research 57, 1–12 (2017).