CASE OF THE MONTH: August 2022
Something bubbling under the surface



Case Presentation
52 year-old male presents with 1-2 years of gradual blurring and dimming of vision from his left eye with acute worsening in the previous 2-3 months
History
PMHx: gonorrhea, chlamydia
- POHx: none
- SHx: immigrated to US from Venezuela in 2001, MSM with numerous high-risk sexual encounters, poor access to medical care
- FHx: none
- Allergies: none
- Rx: none
- ROS: (+) intermittent left ear tinnitus, (+) remote painful oral ulcers, (+) migratory rashes, (+) rare left upper extremity numbness
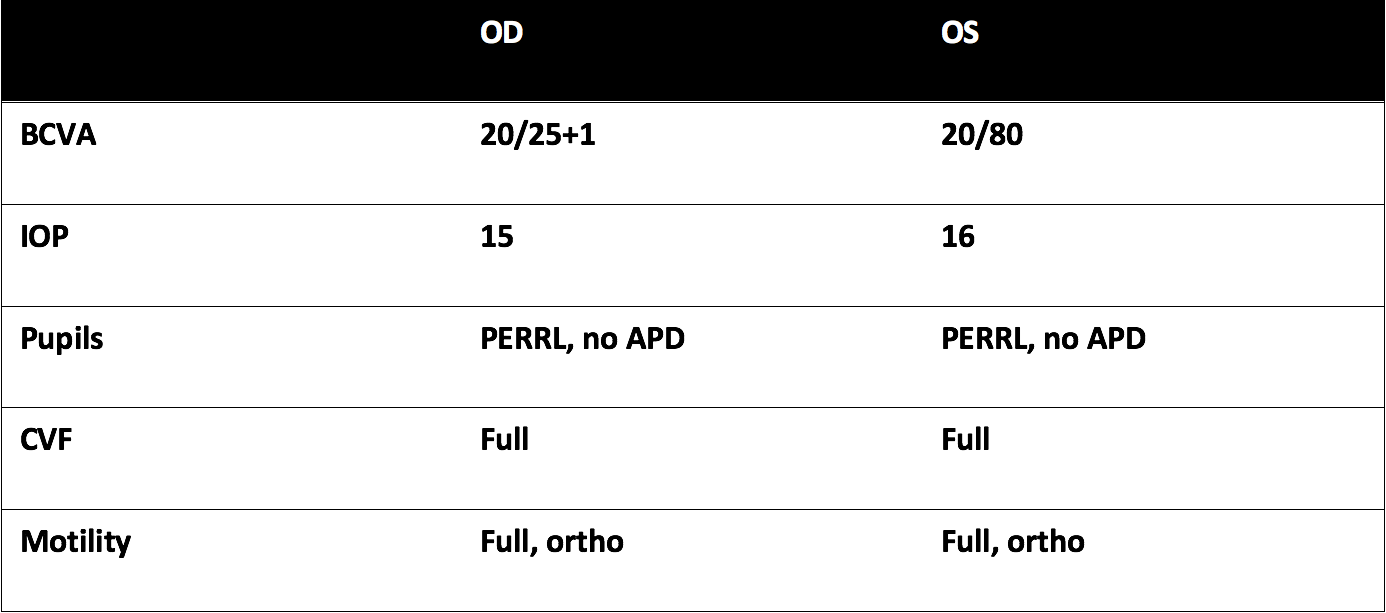
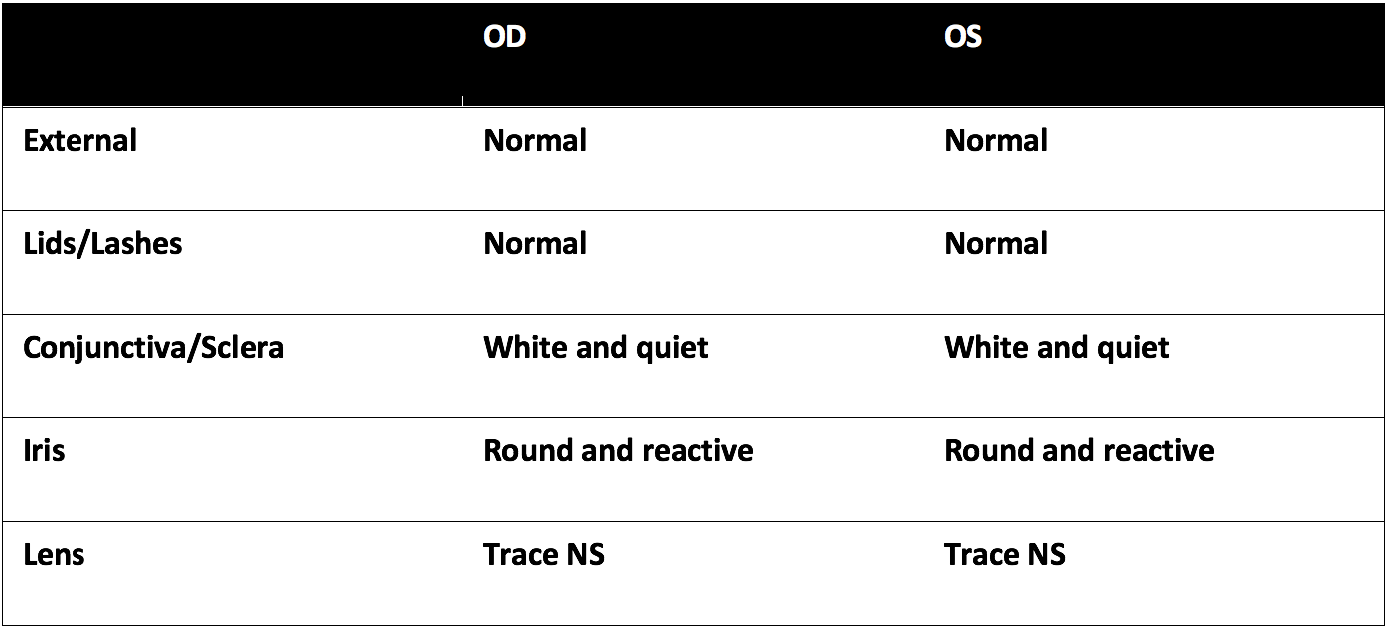
Exam
Summary of Findings
- 52 year-old male presents with 1-2 years of gradual blurring and dimming of vision from his left eye with acute worsening in the previous 2-3 months, in addition to intermittent left ear tinnitus, remote painful oral ulcers, migratory rashes, rare left upper extremity numbness
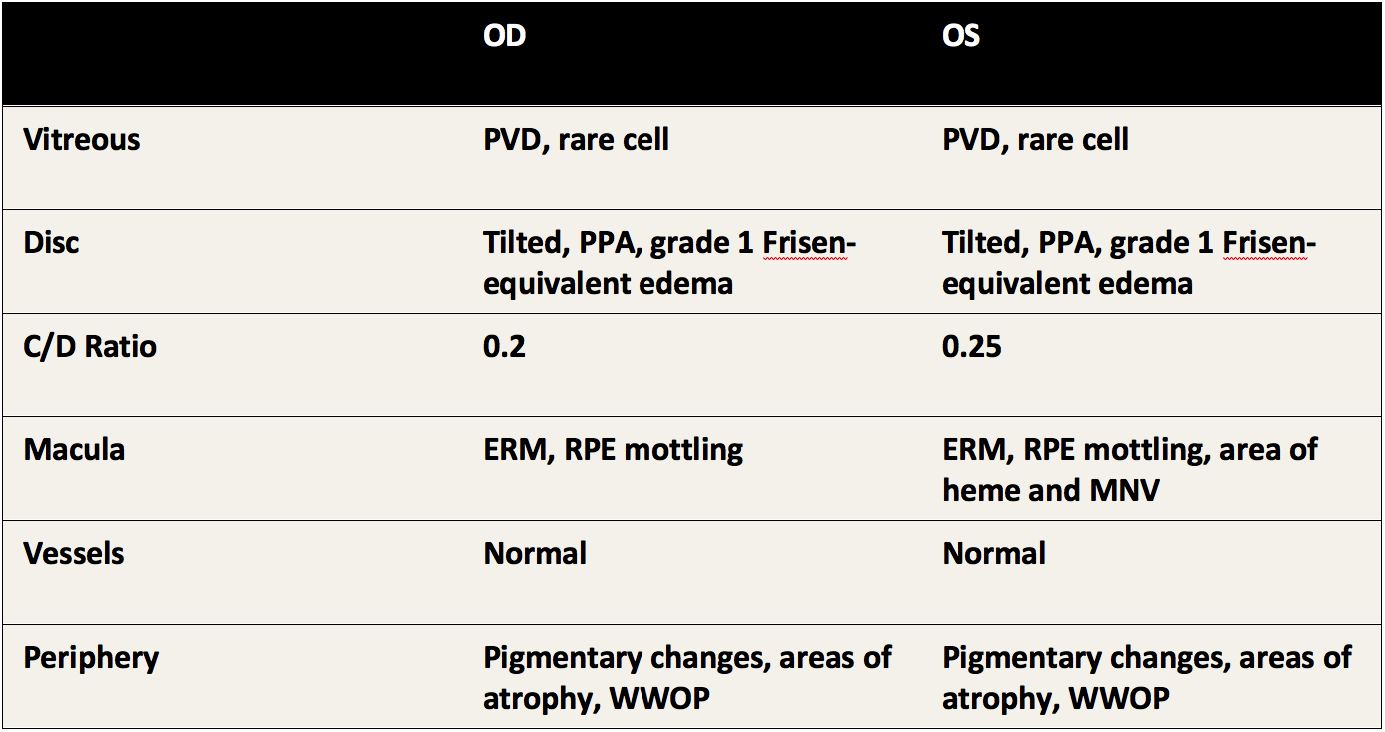
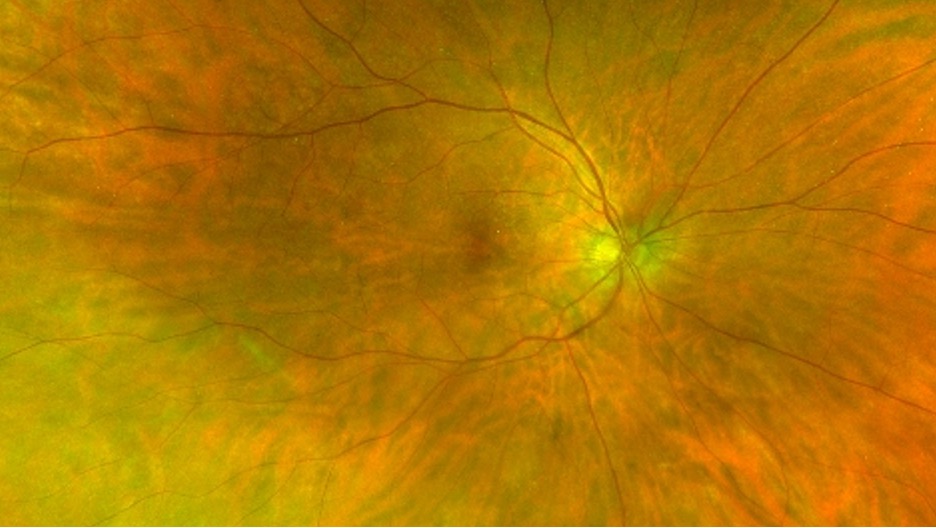
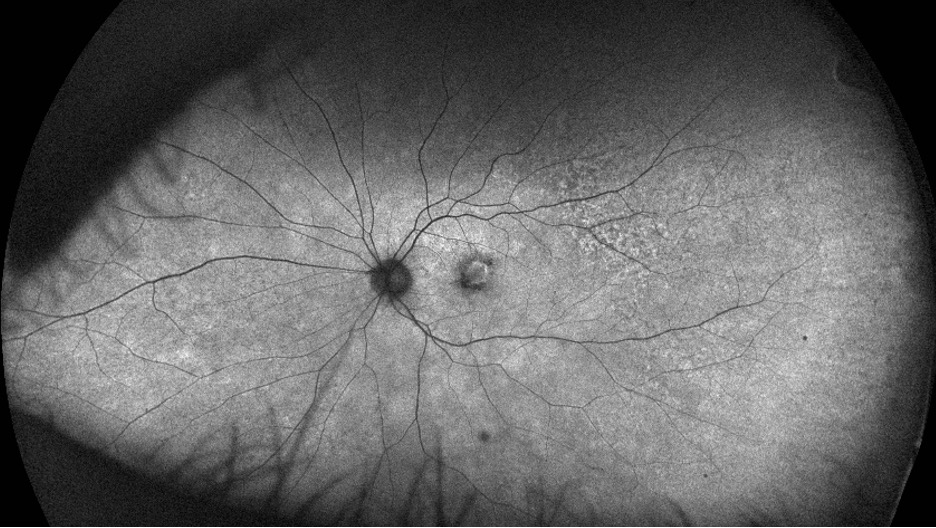
- Funduscopy: bilateral low grade posterior vitreous cell, subtle disc edema, mottling of the retinal pigment epithelium (RPE), and left eye macular hemorrhage
- OCT: epiretinal membrane, subretinal hyperreflective material and fluid suggestive of macular neovascularization (MNV) left eye, and areas of attenuated ellipsoid signal extrafoveal without markedly thickened choroid or subretinal fluid
- FA: mild late disk leakage, peripheral vascular sheathing, window defects, MNV with leakage left eye
Mechanism and differential diagnosis (inflammatory CNV/MNV)
- Degenerative disruption in Bruch's membrane-RPE complex and/or inflammatory-mediated angiogenesis
- Neovascular buds proliferate through damaged RPE-Bruch's complex and leak fluid into subretinal space
- Varied differential summarized in above table[1]
- Elevated suspicion for treponemal disease given pattern of outer retinal atrophy and systemic findings
Workup
Broad uveitis workup sent:
- CBC, CMP, ESR, CRP, ANA, ANCA, ACE, Lysozyme, RF, Anti-dsDNA, HLA-B27, RPR, FTAbs, Quant-gold, Lyme, Toxo IgG/IgM, HLA DR-4, Smith Ab, Anti-ccp, Anti-centromere, Anti-RNP, HIV, West Nile, Coxsackie
- RPR reactive (titer 1:128 - highly positive)
- T. Pallidum Ab reactive
Treatment & clinical course
- Hospital admission for cerebrospinal fluid studies (negative) and IV penicillin for chronic posterior syphilitic uveitis
- ~2 weeks after penicillin treatment, started monthly bevacizumab for secondary MNV with improvement and eventual resolution of fluid and flow within MNV complex, replaced by area of fibrosis
- Visual acuity improved to 20/30+ OS
- After penicillin treatment: Onset of new transitory outer retinal microcysts OU, accompanied by underlying increased transmission suggestive of RPE disruption. Lesions appeared and disappeared spontaneously without resultant atrophy. Ongoing for at least 6 months after initial penicillin treatment
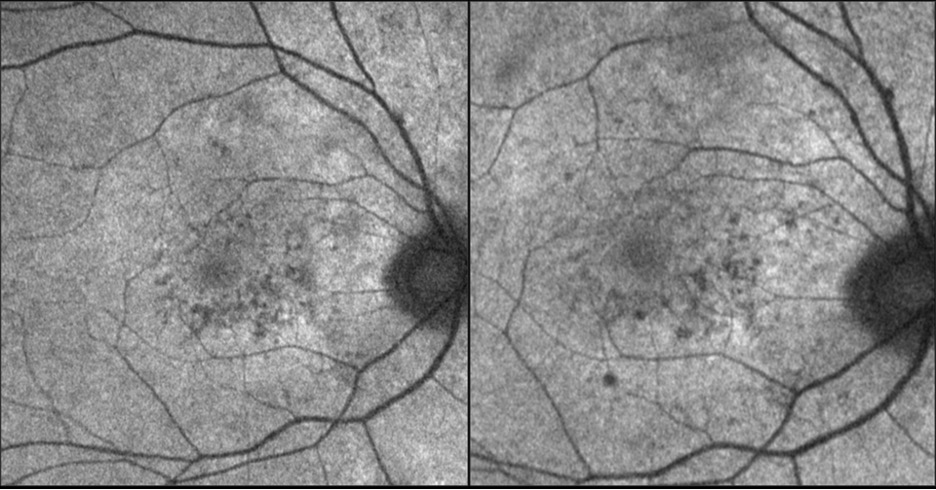
Serial autofluorescence demonstrating transitory nature of outer retinal microcysts, hypo-FAF in these images
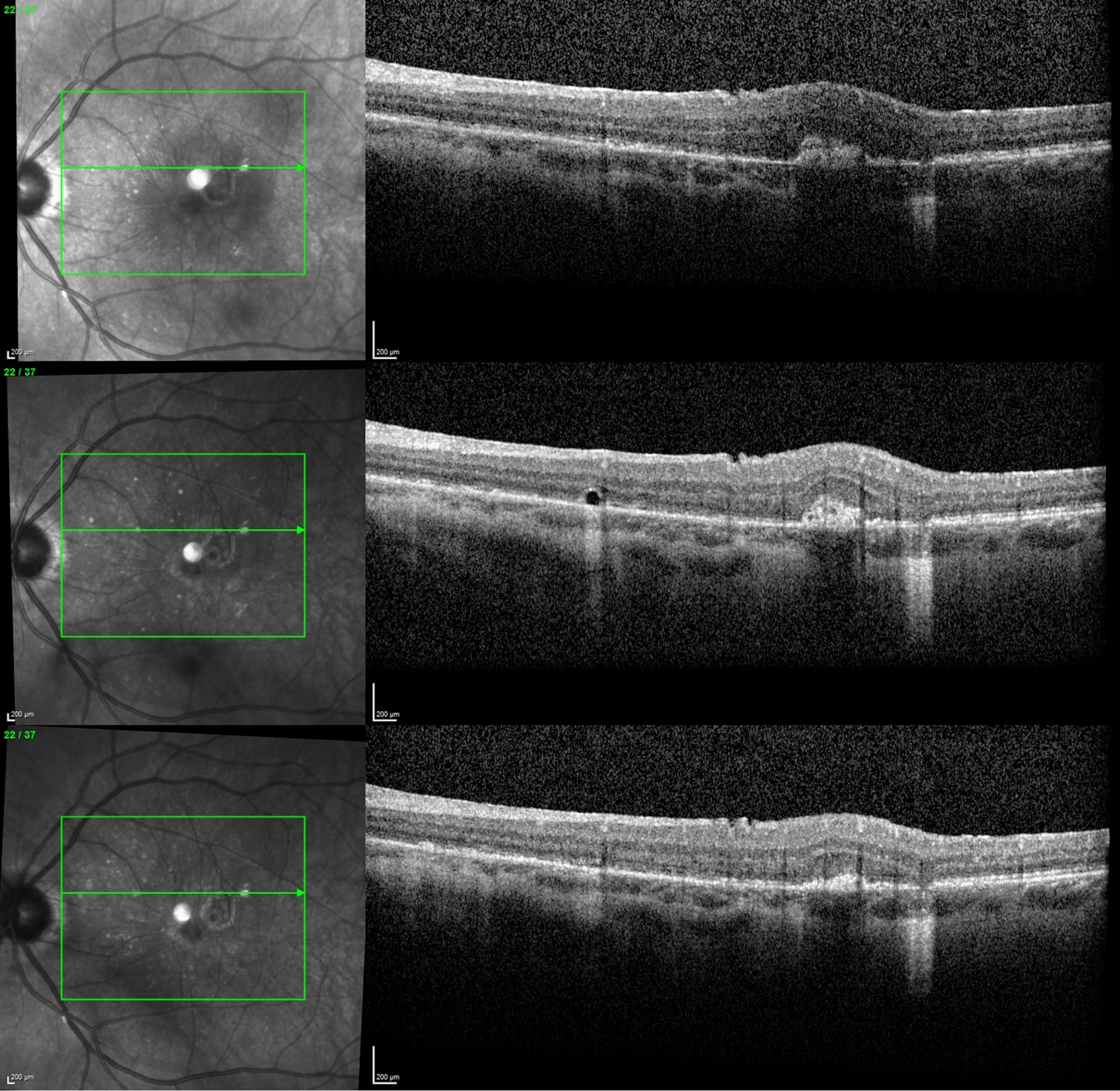
Serial registered OCT OS at relative timepoint 2 weeks, 5 weeks, 9 weeks status-post IV penicillin (also capturing regression of MNV complex)
Discussion
- Treponemal disease predisposing to secondary inflammatory MNV is rare, but documented[2][3]
- Anecdotally MNV has demonstrated good response to combination IV penicillin and oral corticosteroid[4]
- However, transitory outer retinal microcysts are a novel finding in the setting of posterior syphilitic uveitis
- Such lesions are reminiscent of “comet” lesions previously diagnosed as a pathognomonic feature of pseudoxanthoma elasticum,[5] variable in appearance[6] but generally associated with disease chronicity,[7] and later described in a case of retinitis pigmentosa[8]
- We similarly posit that chronic smoldering inflammation and initially high burden of disease led to persistent disruption of RPE-Bruch's complex and the formation of “comet-like” lesions in both eyes following penicillin therapy
1. Agarwal A, Invernizzi A, Singh RB, et al. An update on inflammatory choroidal neovascularization: epidemiology, multimodal imaging, and management. J Ophthalmic Inflamm Infect. 2018;8(1):13. Published 2018 Sep 12. doi:10.1186/s12348-018-0155-6
2. Halperin LS, Lewis H, Blumenkranz MS, Gass JD, Olk RJ, Fine SL. Choroidal neovascular membrane and other chorioretinal complications of acquired syphilis. Am J Ophthalmol. 1989;108(5):554-562. doi:10.1016/0002-9394(89)90433-9
3. Giuffrè C, Marchese A, Cicinelli MV, et al. Multimodal imaging and treatment of syphilitic choroidal neovascularization. Retin Cases Brief Rep. 2022;16(1):85-88. doi:10.1097/ICB.0000000000000912
4. Balaskas K, Spencer S, D'Souza Y. Peripapillary choroidal neovascularisation in the context of ocular syphilis is sensitive to combination antibiotic and corticosteroid treatment. Int Ophthalmol. 2013;33(2):159-162. doi:10.1007/s10792-012-9641-2
5. Gass JD. "Comet" lesion: an ocular sign of pseudoxanthoma elasticum. Retina. 2003;23(5):729-730. doi:10.1097/00006982-200310000-00029
6. Murro V, Mucciolo DP, Sodi A, et al. Peripapillary comet lesions and comet rain in PXE-related retinopathy. Graefes Arch Clin Exp Ophthalmol. 2018;256(9):1605-1614. doi:10.1007/s00417-018-4037-2
7. Barteselli G, Viola F. Comet lesions in pseudoxanthoma elasticum: a spectral domain optical coherence tomography analysis. Retina. 2015;35(5):1051-1053. doi:10.1097/IAE.0000000000000396
8. Battaglia Parodi M, Romano F, Bandello F. Comet Lesions in Retinitis Pigmentosa. Retina. 2018;38(7):e46-e47. doi:10.1097/IAE.0000000000002119