CASE OF THE MONTH: April 2025
It's the Little Things

Case 1:
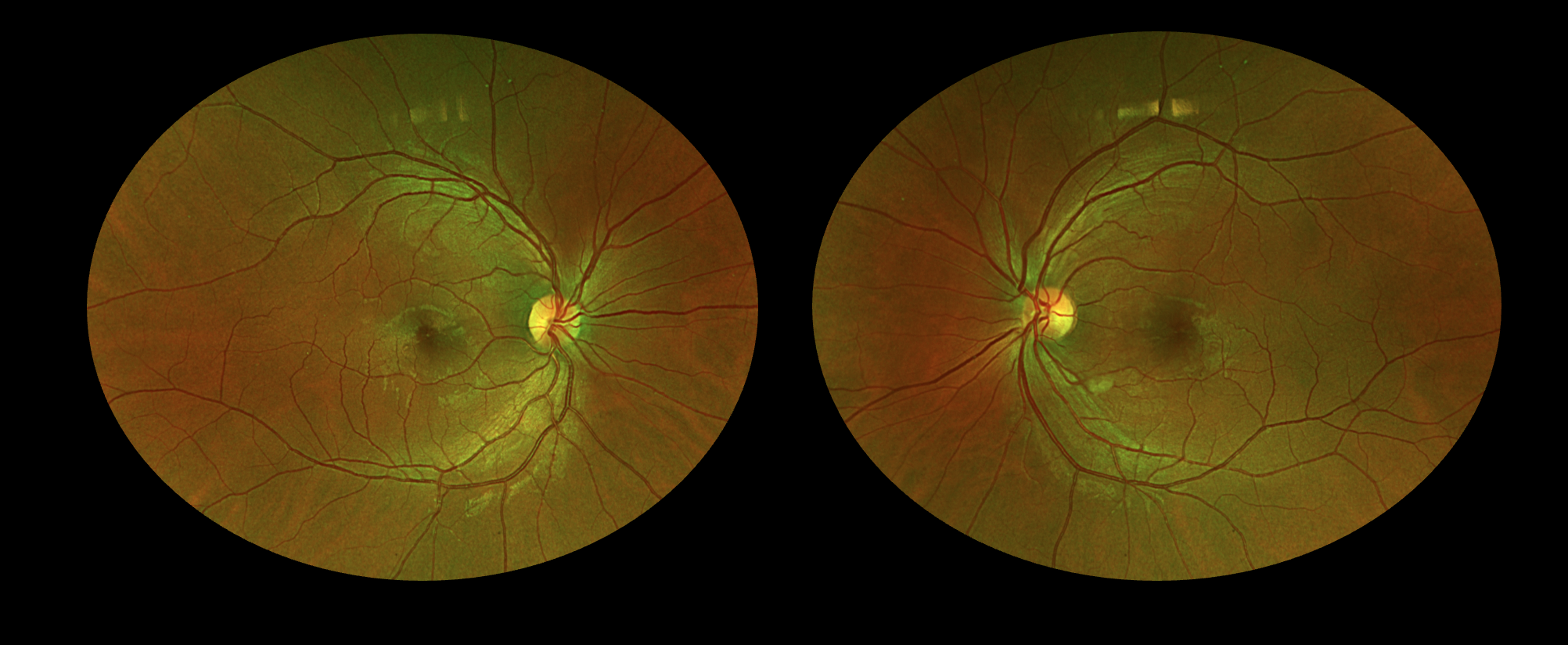
- 29-year-old African American male presenting with central scotomas in the left > right eye
- Started during recent infection with Influenza A
- Completed work up including laboratory testing in the Emergency Department, all of which was negative
- No past medical history
- No medication use
- Visual acuity 20/60 OD, 20/100 OS


Summary of Key Imaging Findings:
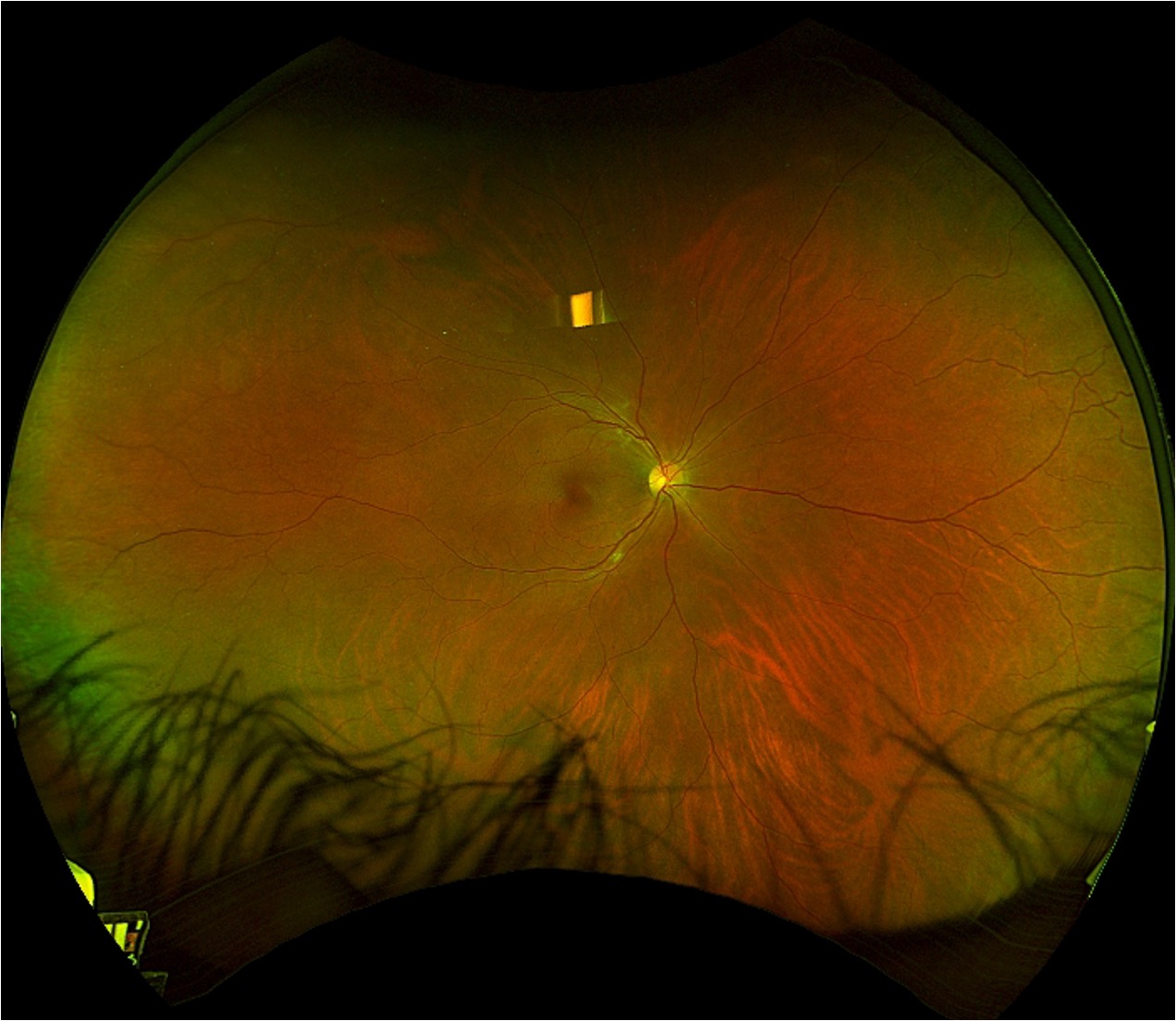
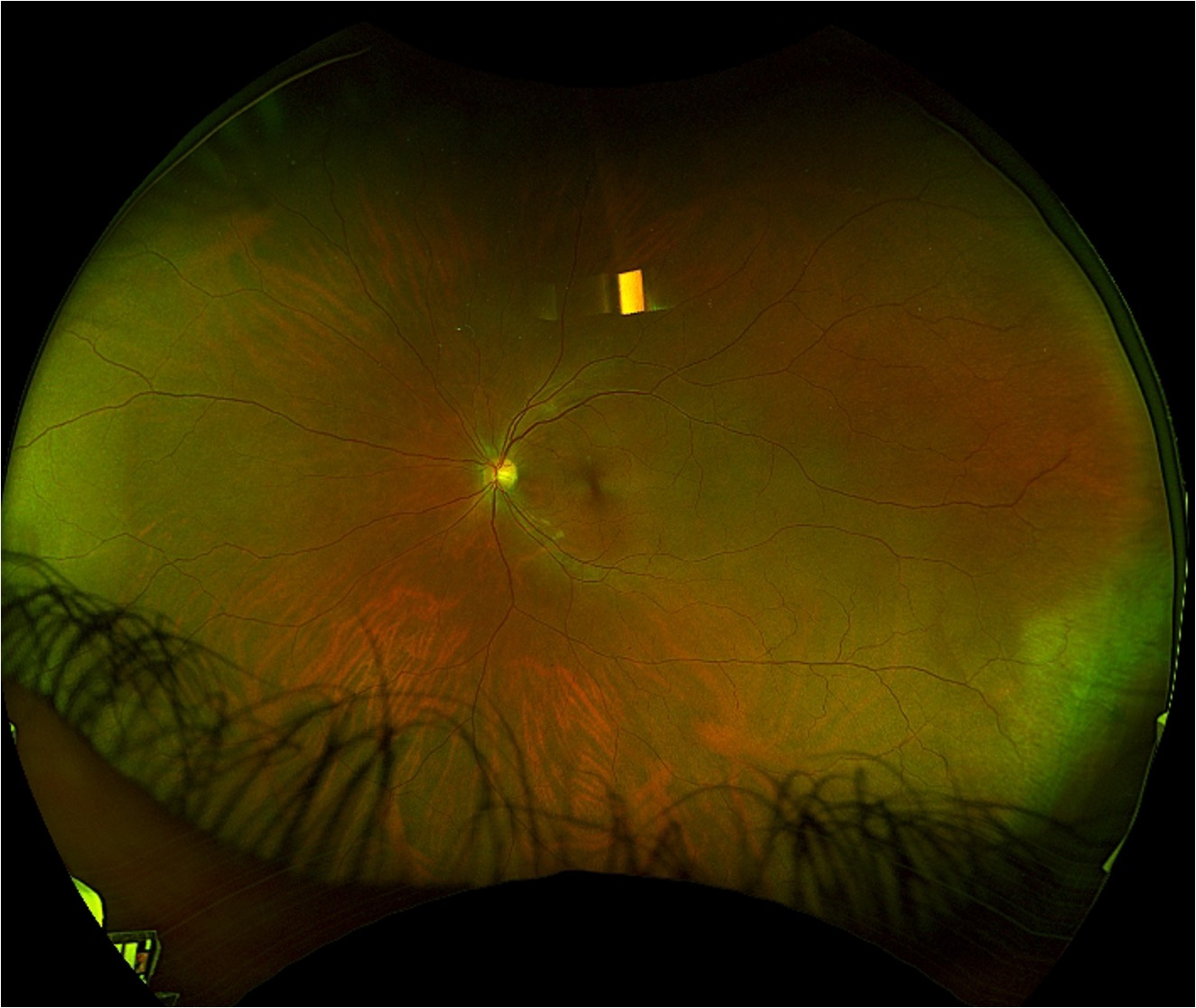
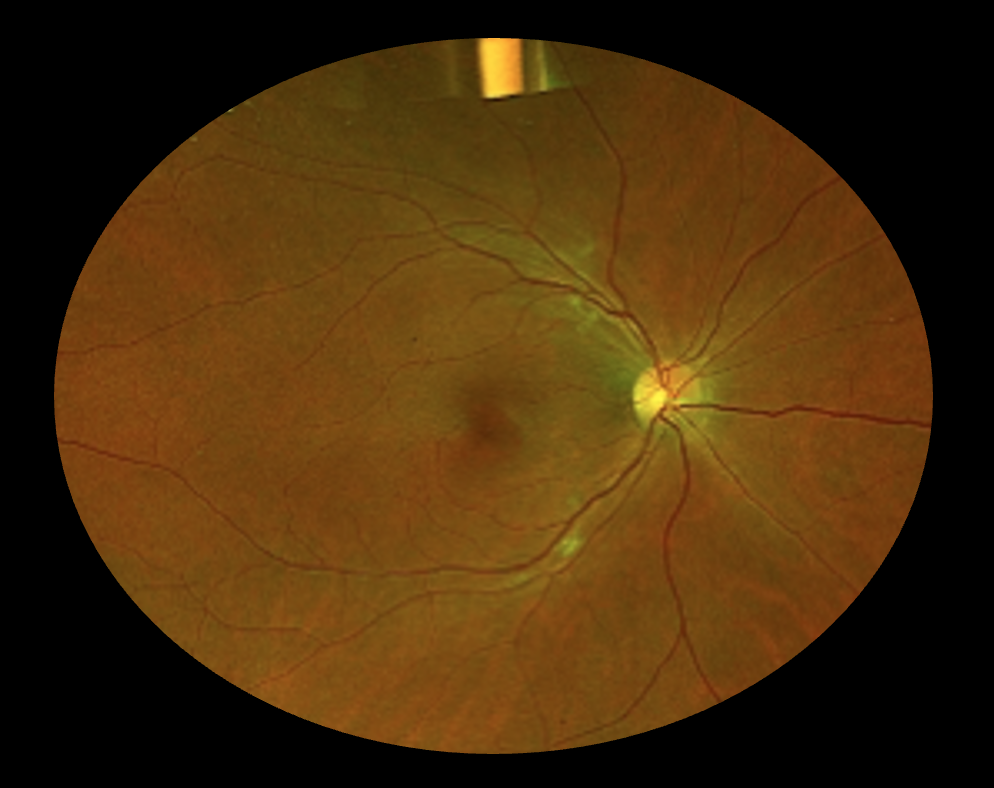
- Fundus photographs demonstrate subtle reddish wedge-shaped parafoveal discoloration in both eyes and cotton wool spots in the left eye.
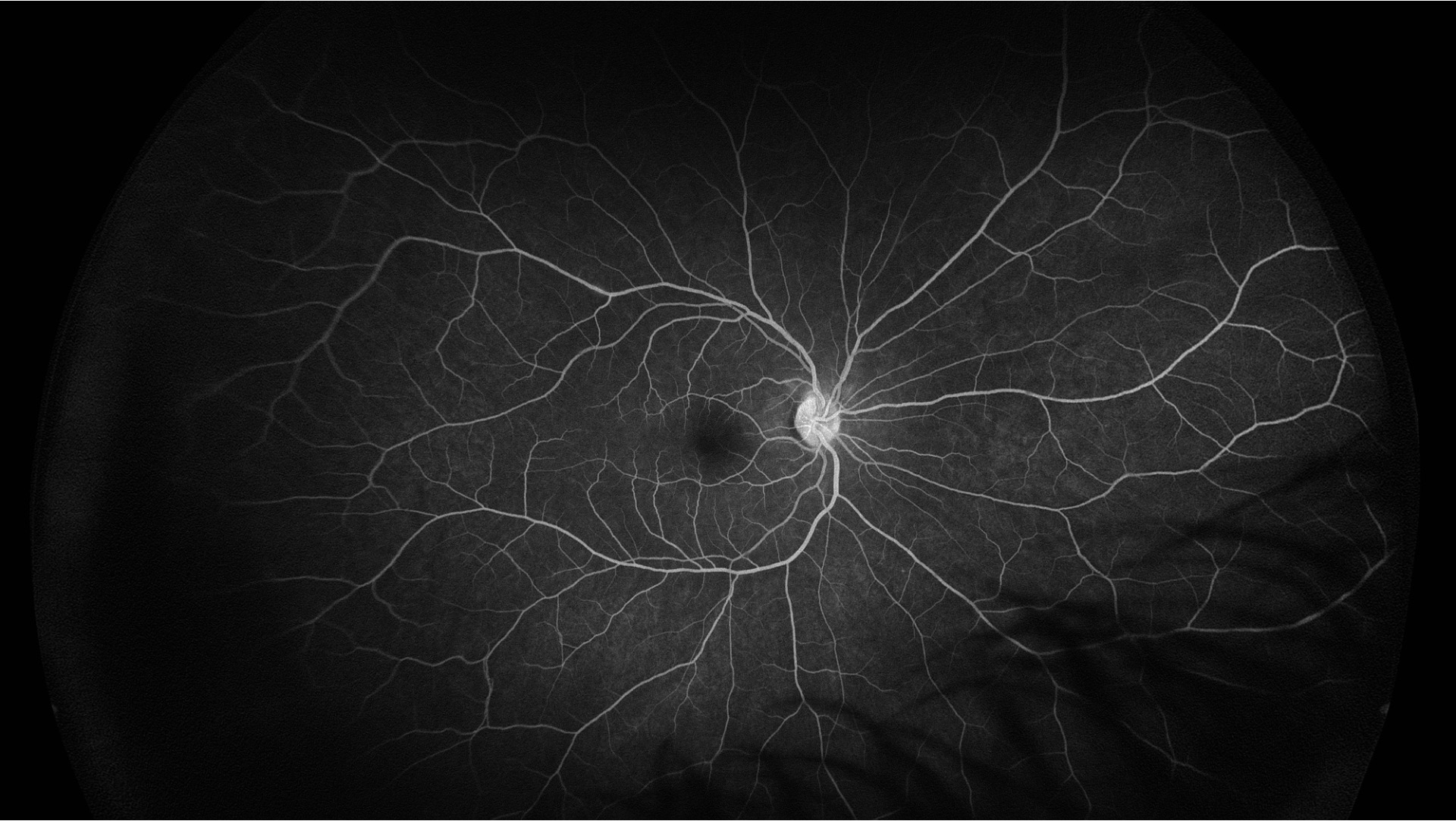
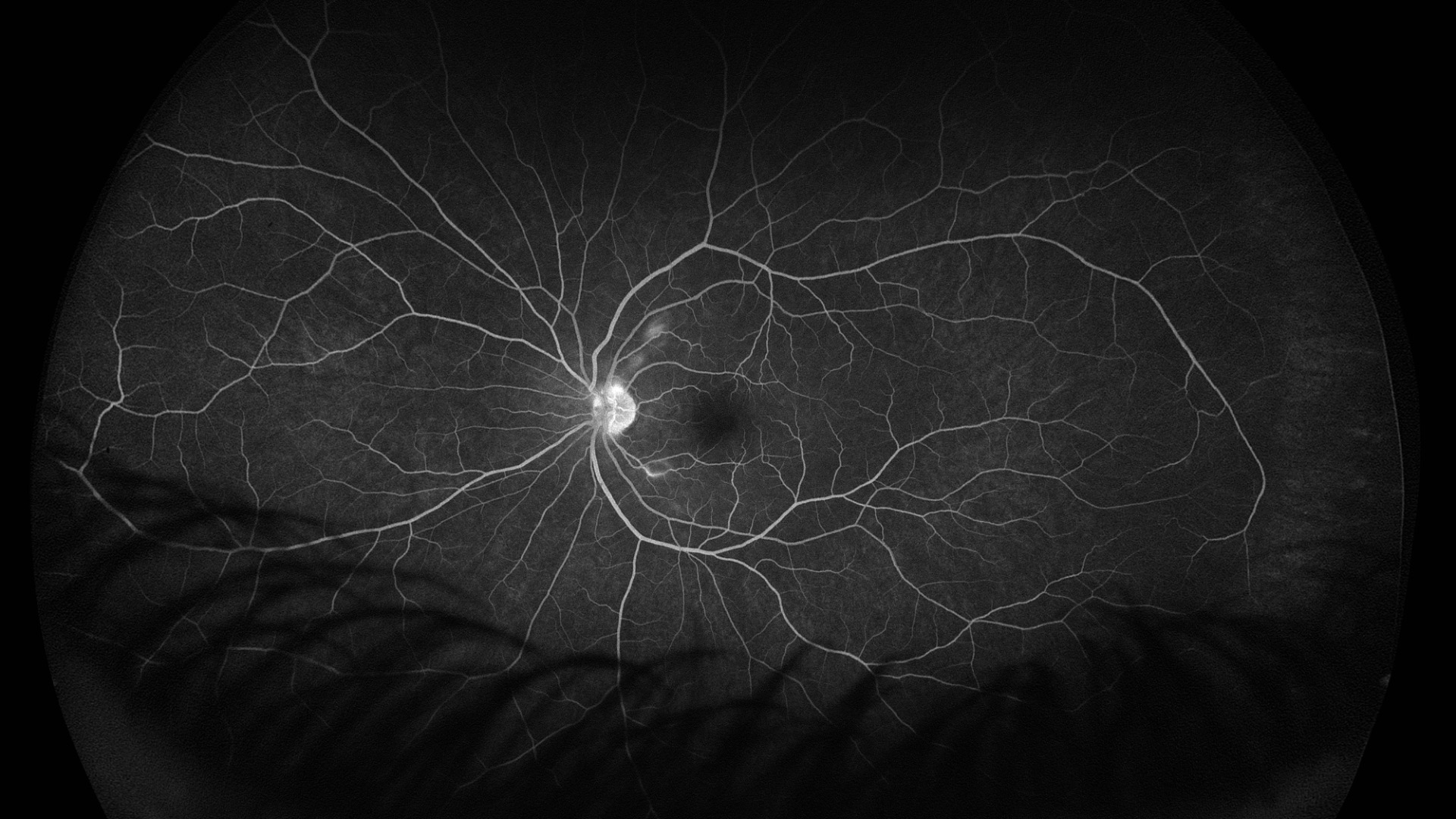
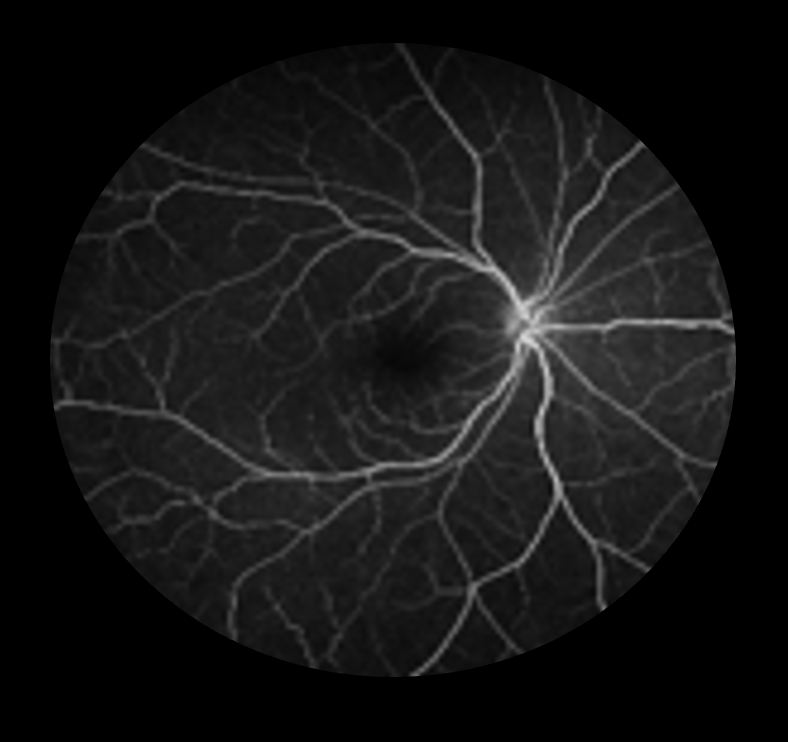
- Fluorescein angiogram of the left eye demonstrates mild perivascular leakage corresponding to the cotton wool spots.
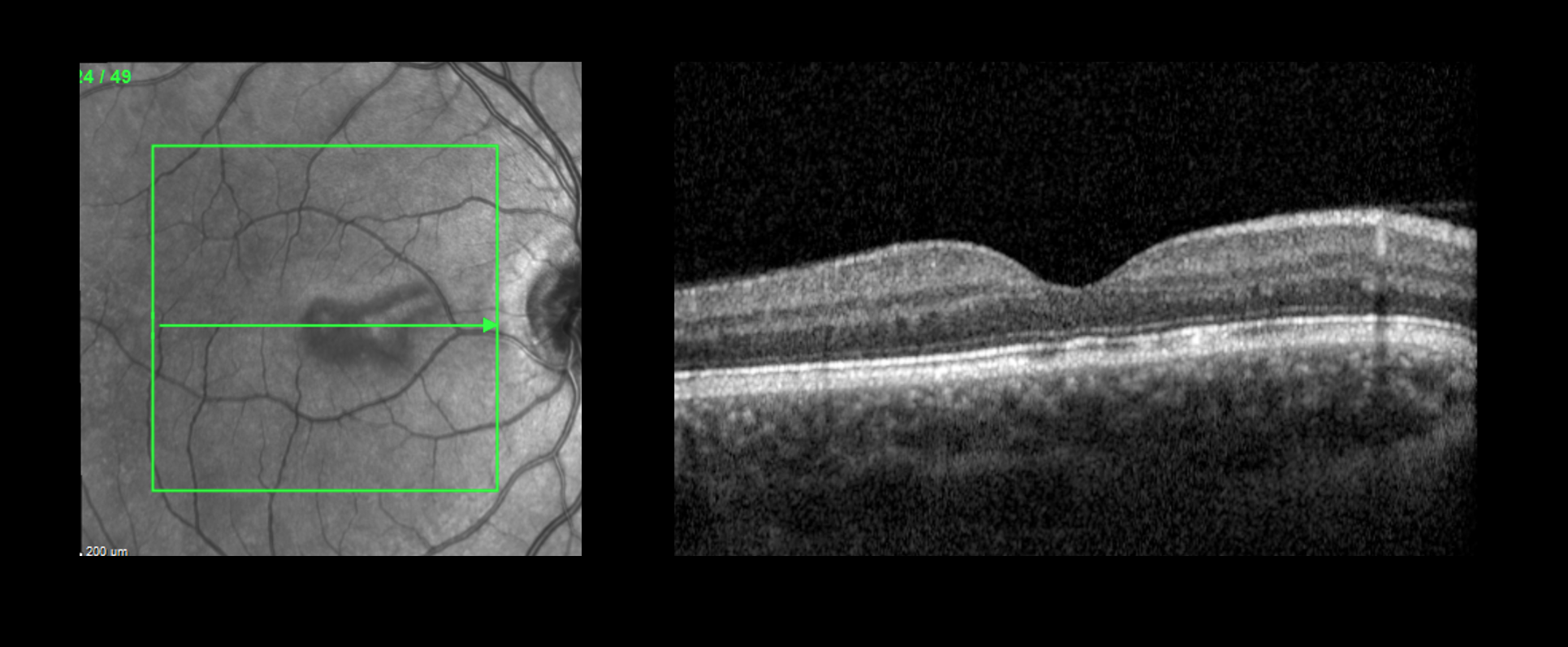
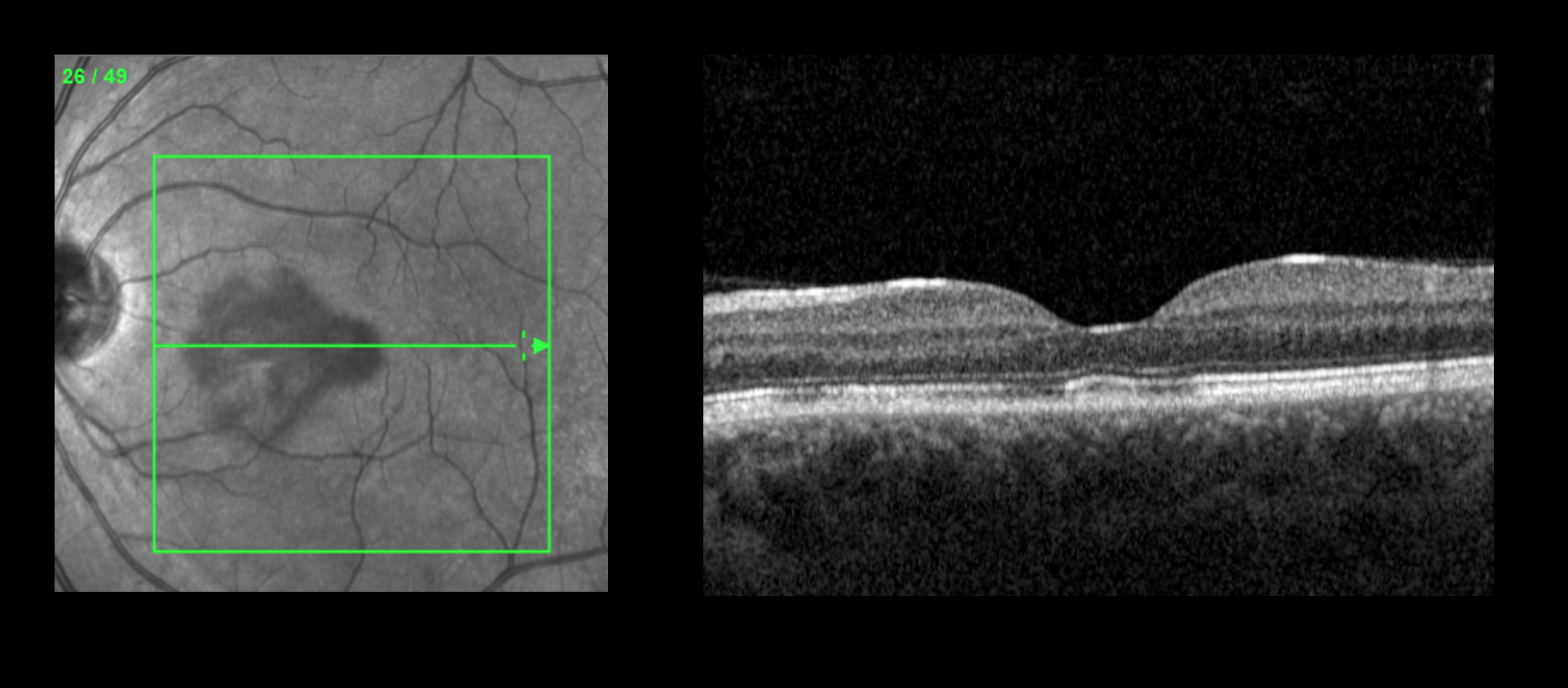
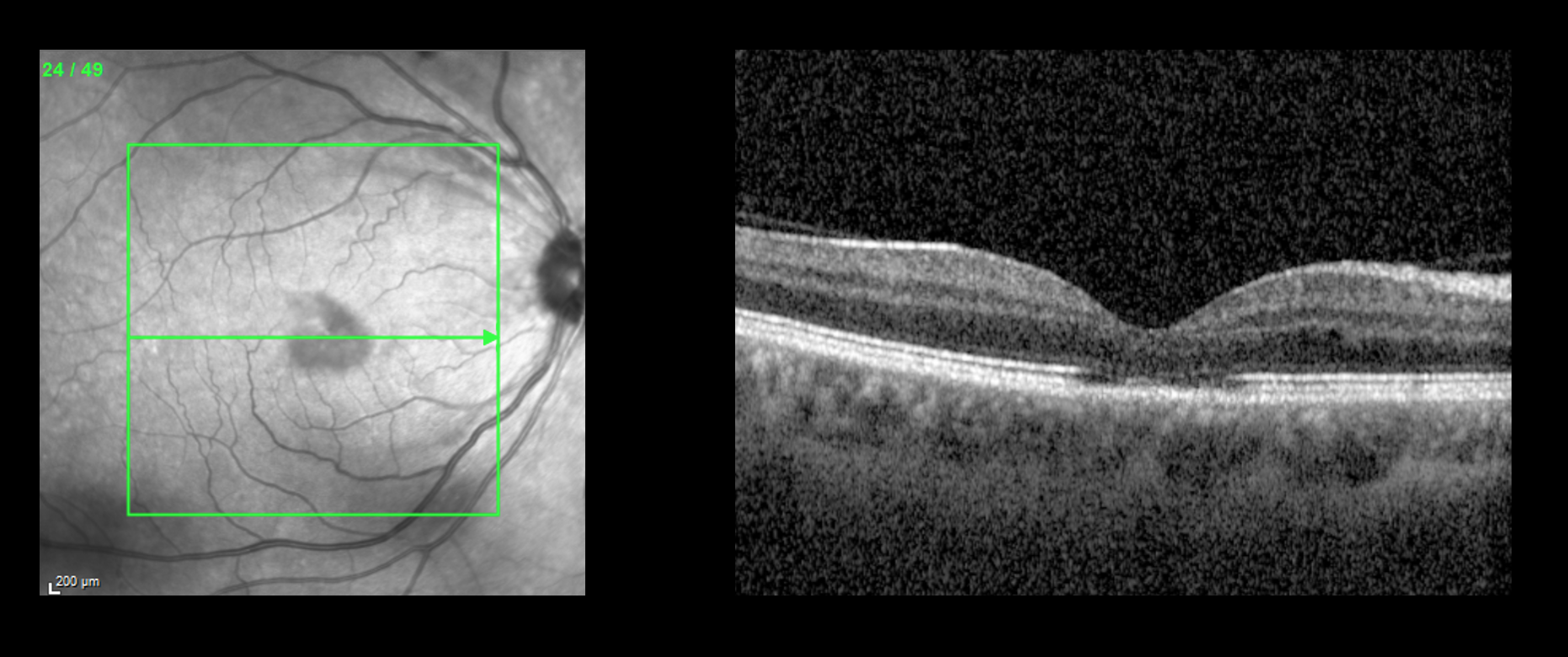
- OCT demonstrates focal outer retinal disruption at the ellipsoid and interdigitation zones and subtle hyperreflectivity in the outer nuclear and outer plexiform layers in both eyes.
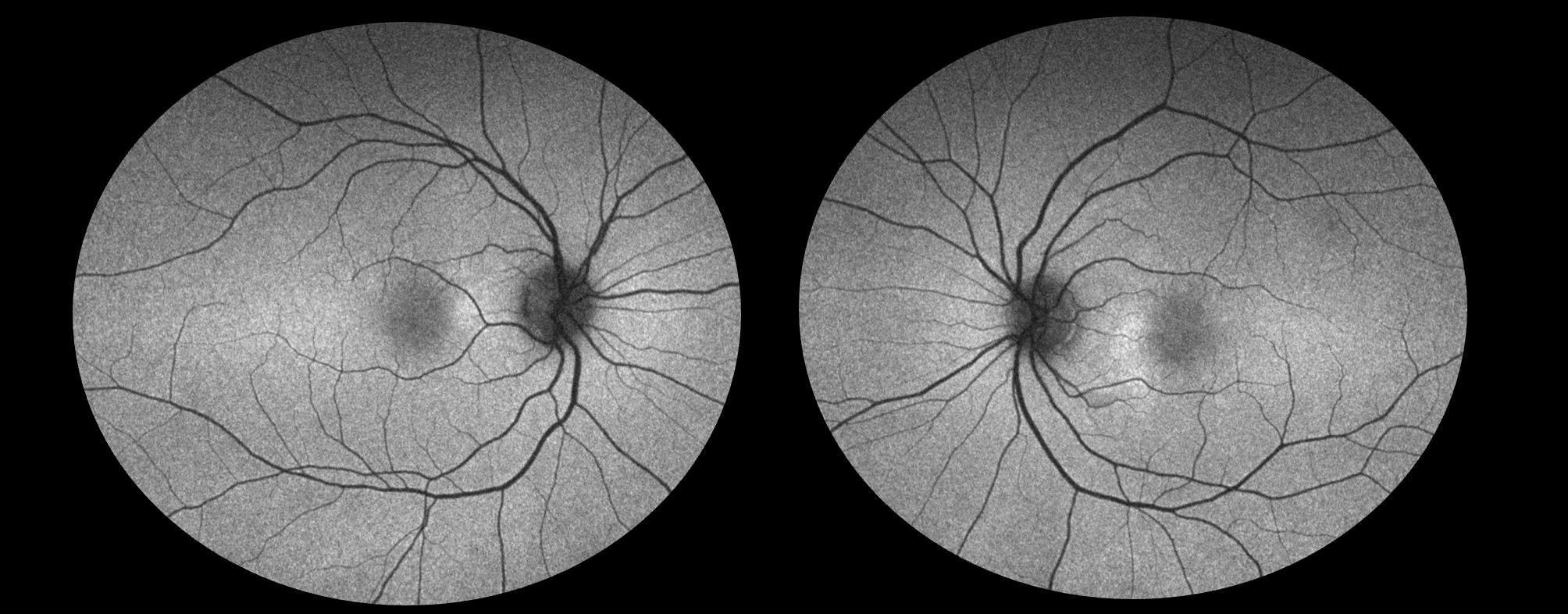
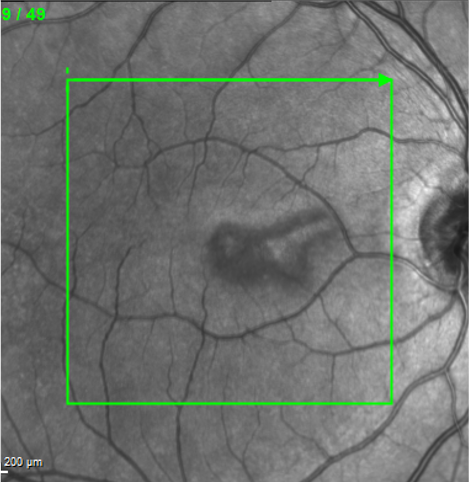
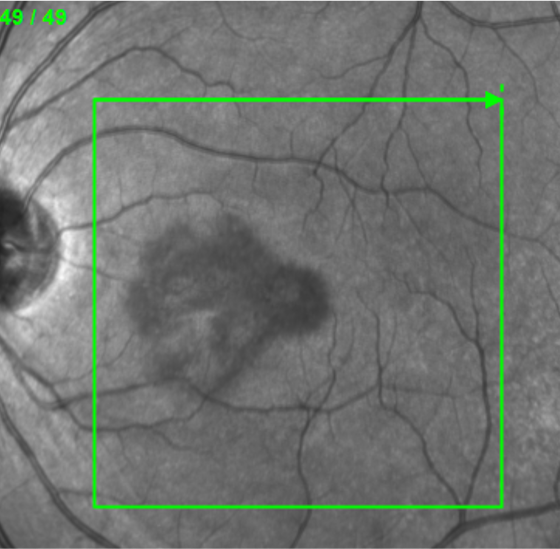
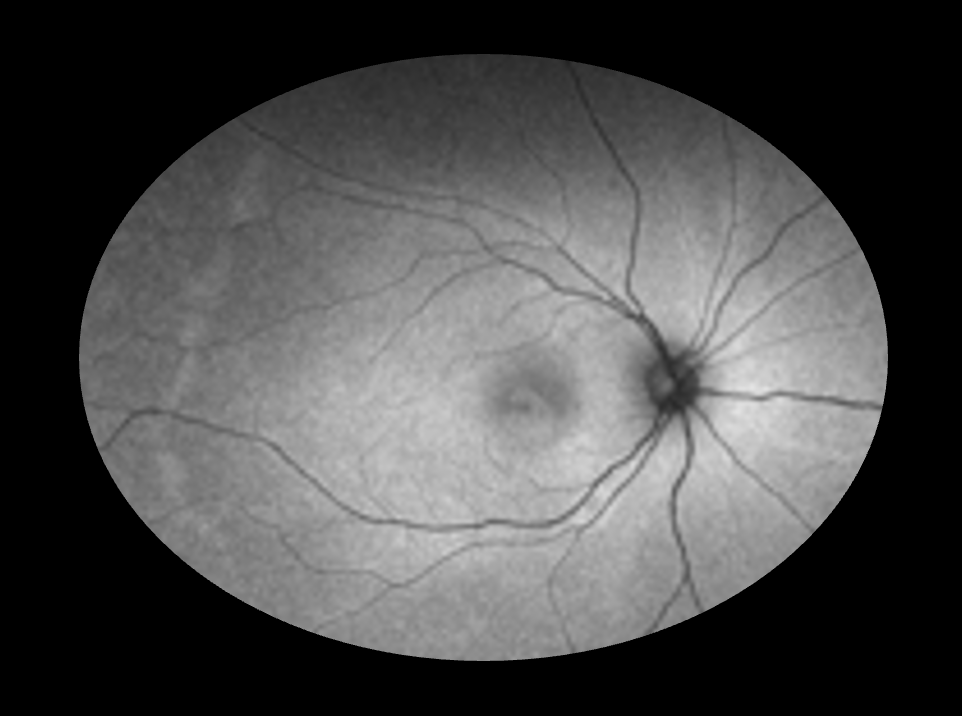
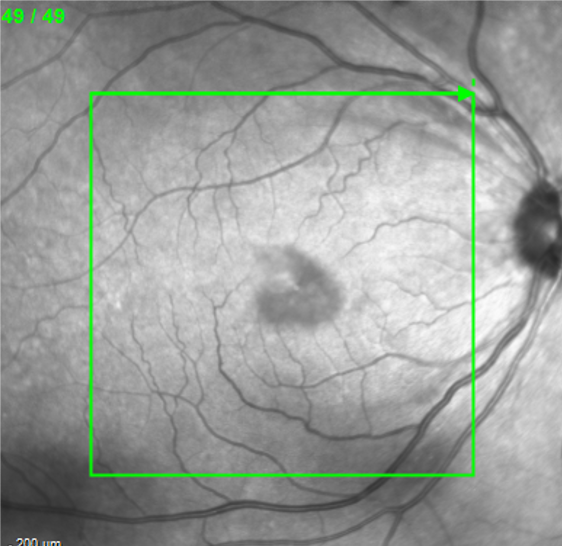
- Near-infrared reflectance images demonstrate wedge-shaped hyporeflective parafoveal lesions pointing toward the fovea in both eyes.
Case 2:
- 48-year-old African American female presenting with right central scotoma during an episode of gastrointestinal virus
- History of severe post-COVID syndrome two years ago
- No other past medical history
- VA 20/30 OD, 20/25 OS


Key Imaging Findings:
- Fundus photographs demonstrate a subtle reddish wedge-shaped parafoveal discoloration in the right eye and cotton wool spots in both eyes.
- OCT demonstrates focal outer retinal disruption at the ellipsoid and interdigitation zones and subtle hyperreflectivity in the outer nuclear and outer plexiform layers in the right eye.
- Near-infrared reflectance (NIR) image demonstrates a wedge-shaped hyporeflective parafoveal lesion pointing toward the fovea in the right eye.
Differential Diagnosis:
- Acute macular neuroretinopathy (AMN)
- Paracentral Acute Middle Maculopathy (PAMM)
- Acute Retinal Pigment Epitheliitis (Krill's disease)
- Multiple Evanescent White Dot Syndrome (MEWDS)
- Acute Posterior Multifocal Placoid Pigment Epitheliopathy (APMPPE)
- Central Serous Chorioretinopathy (CSCR)
- Old inner retinal infarcts
Acute Macular Neuroretinopathy (AMN):
- AMN is an uncommon retinal disorder characterized by distinctive but subtle, wedge-shaped, reddish-brown lesions within the retina, typically oriented with their points directed toward the fovea.
- AMN presents with sudden-onset paracentral scotomas, typically in young women, often bilateral or asymmetric, which correlate to the lesions.
- Because of their subtlety, findings are easily missed without multimodal imaging.
- Hyperreflectivity at the outer plexiform and outer nuclear layers, with disruption of the ellipsoid zone are seen on OCT.
- While the exact cause of AMN remains multifactorial, available evidence supports an underlying microvascular origin.
- AMN is often linked to flu-like illness including COVID-19, fever, oral contraceptive use, vasoconstrictive agents, or systemic hypotension.
- In a major review, Bhavar et al1 report that AMN was bilateral in 54.4% of patients with presenting visual acuity 20/40 or better in 80.8% of eyes. In 5.8% of eyes, lesions could only be identified on NIR imaging. The majority of patients were female (84.2%) and median age at presentation was 26 years. Most patients (47.5%) reported recent infection or febrile illness. A further 35.6% reported oral contraceptive use.
- Imaging findings and etiologies suggest AMN originates from an ischemic event in the retinal deep capillary plexus.2,3 AMN lesions have been also been associated with cotton wool spots, retinal hemorrhages, and cystoid macular edema.1,4
- Prognosis is variable, with some patients reporting complete resolution of scotomas, while others experience only partial or no resolution.
Back to our cases:
- Both patients had negative systemic work-ups
- Scotomas have improved but not resolved in both patients at 3-4 months of follow up
References
Bhavsar KV, Lin S, Rahimy E, et al. Acute macular neuroretinopathy: A comprehensive review of the literature. Surv Ophthalmol. 2016;61(5):538-565.
Turbeville SD, Cowan LD, Gass JD. Acute macular neuroretinopathy: a review of the literature. Surv Ophthalmol. 2003;48(1):1-11.
Cabral D, Ramtohul P, Zatreanu L, et al. Deep Capillary Plexus Features in Acute Macular Neuroretinopathy: Novel Insights Based on the Anatomy of Henle Fiber Layer. Invest Ophthalmol Vis Sci. 2022;63(13):4.
Groat CL, Ellis BD, Leys MJ. A Unique Case of Acute Macular Neuroretinopathy Associated with Cotton Wool Spots and Intraretinal Fluid. Retin Cases Brief Rep. 2016;10(1):26-31.