CASE OF THE MONTH: October 2024
Chronic Red Eye


Case:
Case Presentation
A 67-year-old male presents with a three month long history of blurred vision and photophobia in the right eye. He endorses a history cataract surgery nine months prior with an outside eye clinic.
History
- POHx: Uncomplicated cataract surgery, both eyes, RK, both eyes
- SHx: Lives with wife, no pets
- FHx: None
- Allergies: None
- Rx: None
- ROS: Photophobia
PMHx: Hypertension
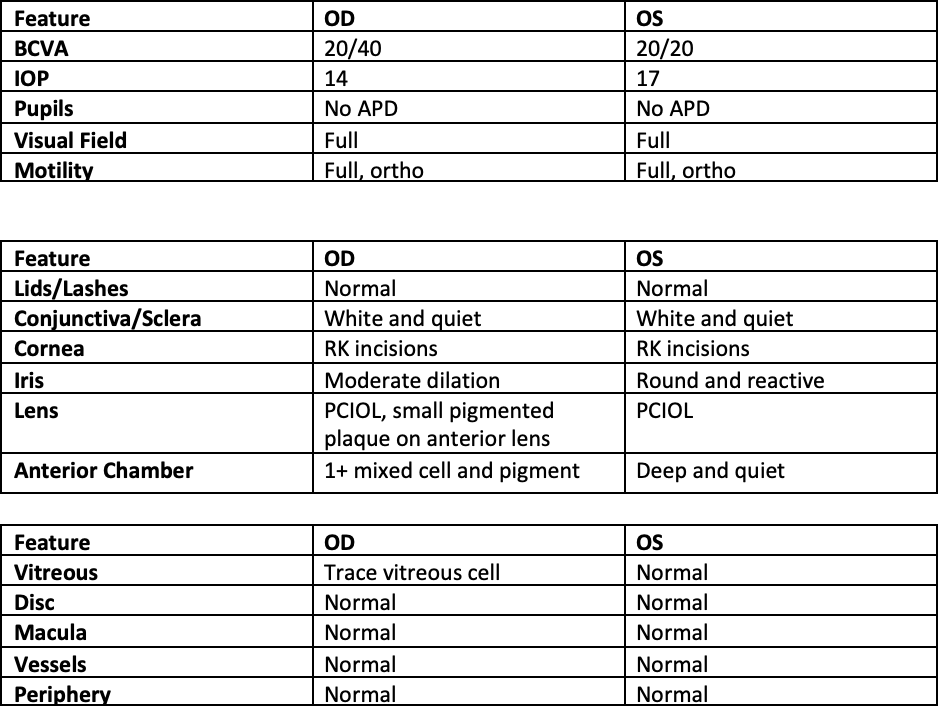

Summary of Findings
- The patient was referred for photophobia, iritis that recurred with each topical prednisolone acetate taper, and blurred vision. His ocular history was significant for cataract surgery eight months prior without complications.
- Examination revealed 1+ mixed anterior cell and pigment, and a small pigmented lens deposit on the anterior lens. The iris dilated poorly and required multiple rounds of drops. Gonioscopy done prior to dilation showed no evidence of retained lens fragments. Posterior examination was unremarkable besides trace vitreous cell.
- Social history and medical history was unremarkable besides a history of hypertension.
- Given the concern for chronic endophthalmitis, an aqueous humor sample was taken and sent for gram stain and culture; gram stained showed no polymorphonuclear leukocytes, no epithelial cells, and no organisms. A broad uveitis work up was initiated as well.
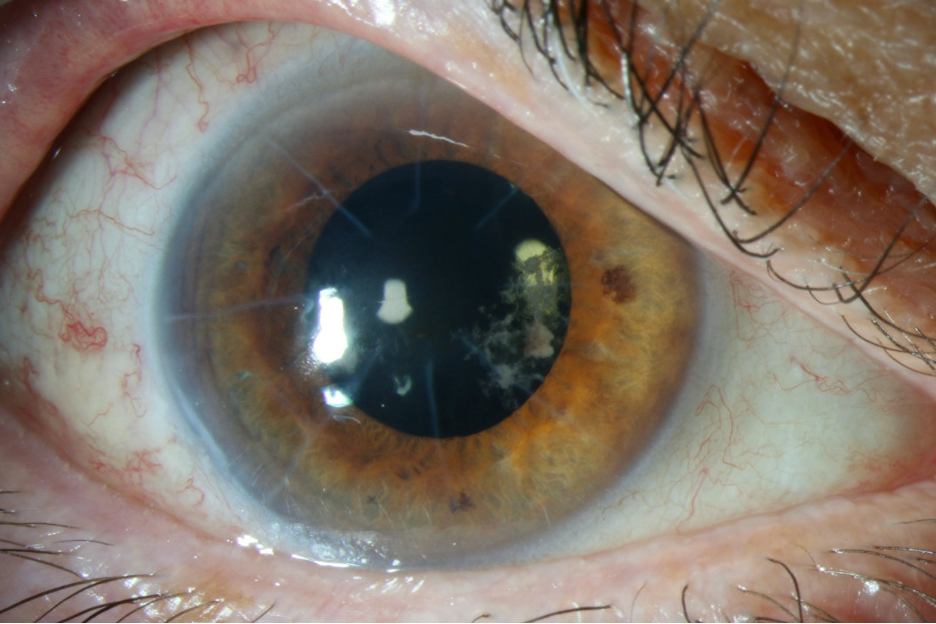
- Given the lack of growth, the patient was placed back on topical steroids and with recurrent taper, the patient presented with a worsening pigmented plaque on the capsule, with worsening inflammation in the anterior chamber. (Figure 1)
- With the worsening inflammation the patient underwent a repeated anterior chamber paracentesis with aqueous humor sent for universal PCR testing at the University of Washington. This revealed Moraxella osloensis on PCR testing. The patient also received intravitreal vancomycin and ceftazidime.
- 1 day later, the patient presented with an impressive hypopyon. (Figure 2) It was thought that the hypopyon was secondary to inflammation from the death of the Moraxella osloensis organism. The patient was treated with topical prednisolone acetate every 1 hour and atropine twice a day and followed closely. After two days, the hypopyon started to resolve and the patients eye pain improved.
- The patient was followed closely with resolution of intraocular inflammation.
- At his last follow up visit his vision improved to 20/25, and there has been no recurrent inflammation of topical steroid drops.
Mechanism and differential diagnosis
Work up
- The main differential diagnoses include chronic infection versus non infectious uveitis
- A broad uveitis work up sent, including: ACE, muramidase, QuantiFERON, syphilis IgM/IgG, T. universal PCR including testing for bacterial, fungal and viral etiologies. A chest CT, brain MRI with and without contrast were also performed. All testing returned negative besides the universal PCR for bacteria.
Treatment and clinical course
- The patient was treated with intravitreal vancomycin and ceftazidime, as well as topical oral prednisolone acetate drops every hour, with improvement in symptoms.
Discussion
- Chronic endophthalmitis can be a difficult condition to treat. (1)
- It presents at least six weeks after intraocular surgery and can masquerade as non infectious uveitis. It occurs in less than 1% of cases undergoing cataract surgery. (1,2)
- The entry of the organism can occur through multiple avenues, including irrigation, surgical instruments, and the placement of the lens on various surfaces. (1)
- Several clues can point towards this diagnosis including recurrent inflammation after intraocular surgery, poor iris dilation, and plaques on the lens capsule or lens. (3)
- In certain cases, the inflammation may persist after intravitreal antibiotics which may necessitate the removal of the lens capsule complex; this is thought to be secondary to a biofilm forming on the lens.
- Diagnosis can be done through the aspiration of aqueous humor and performing analysis through gram stain, culture, and PCR. The highest yield comes from sampling the plaque deposits on the lens. (1)
- The varied presentations of chronic endophthalmitis makes it difficult to establish a singular treatment protocol. Various reports have shown success with intravitreal antibiotics, pars plana vitrectomy with intravitreal antibiotics, or vitrectomy with antibiotics and the removal of the lens/bag complex. (4)
References
1. Maalouf F, Abdulaal M, Hamam RN. Chronic postoperative endophthalmitis: a review of clinical characteristics, microbiology, treatment strategies, and outcomes. Int J Inflam. 2012;2012:313248. doi: 10.1155/2012/313248. Epub 2012 Feb 22. PMID: 22550607; PMCID: PMC3328945.
2. Lemley CA, Han DP. Endophthalmitis: a review of current evaluation and management. Retina. 2007;27(6):662–680.
3. Samson CM, Foster CS. Chronic postoperative endophthalmitis. International Ophthalmology Clinics. 2000;40(1):57–67.
4. Clark WL, Kaiser PK, Flynn HW, Belfort A, Miller D, Meisler DM. Treatment strategies and visual acuity outcomes in chronic postoperative Propionibacterium acnes endophthalmitis. Ophthalmology. 1999;106(9):1665–1670.