CASE OF THE MONTH: Q3 2025
Insidious Floaters: A Case of Ocular Amyloidosis


CHIEF COMPLAINT
- 44-year-old man reports floaters and blurry vision OU for 5 years
HISTORY OF PRESENTING ILLNESS
- S/p PPV OD 1 year prior to presentation
- Following PPV OD, floaters and blurry vision improved for 2 weeks, then worsened
- Pathology from PPV OD showed small lymphocytes within a background of amorphous material, no bacterial or fungal growth on cultures
- S/p STK OS 3 months prior to presentation without improvement in symptoms
- Systemic work up (including ANA, ANCA, RF) was unremarkable
ADDITIONAL INFORMATION
- Review of Systems: Negative
- Ocular Medications: None
- Past Ocular History: Unremarkable
- Medical History: Unremarkable
- Family History: Unremarkable
EXAMINATION
- VA: 20/50 OD, CF OS
- IOP: 16 OD, 44 OS
- Pupils: Round and reactive without APD OU
- C/S: White and quiet OU
- Cornea: Clear without KP OU
- AC: Deep and quiet OU
- Iris: Normal without PS OU
- Lens: White deposits on the posterior lens capsule OU
- Anterior vitreous: Glass wool-like fluffy white vitreous opacities OU
IMAGING
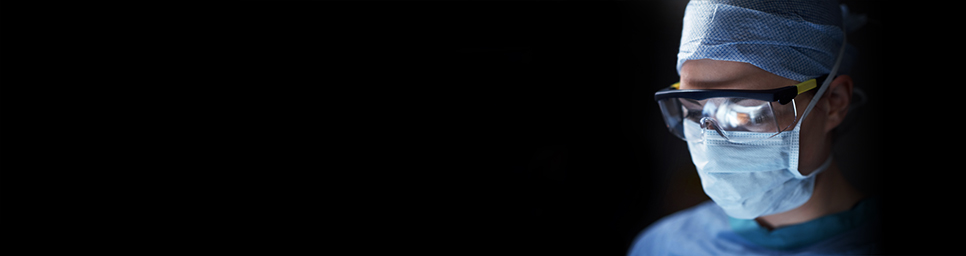
Slit lamp photography of both eyes showing the posterior lenticular deposits with glass wool-like vitreous opacities in the anterior vitreous.
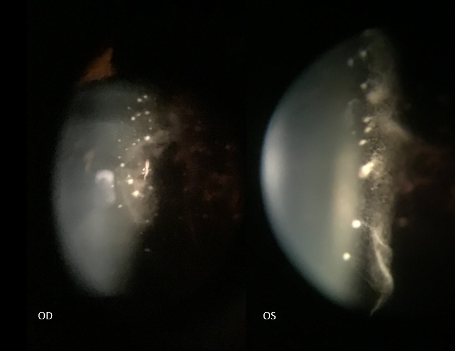
Fundus photography of both eyes showing media opacity in both eyes.
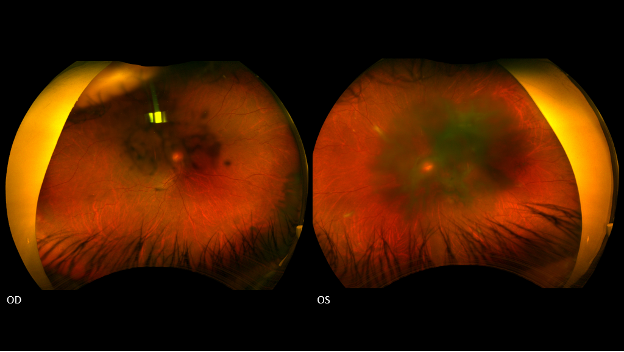
Detailed fundus photography of the right eye depicts white deposits (white arrows) along the peripheral vasculature.
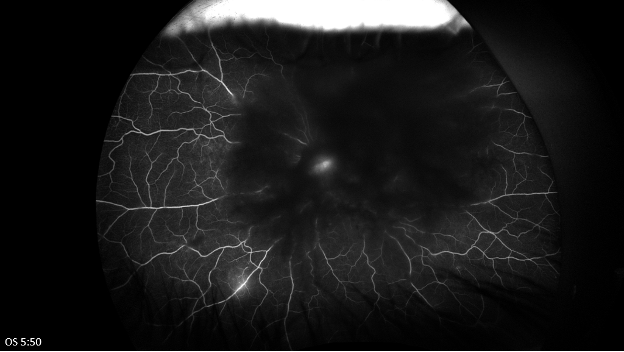
Late phase fluorescein angiography of both eyes shows central blockage in both eyes from lenticular and vitreous opacities. In the left eye there is possible leakage from the optic disc and late venous leakage inferiorly.
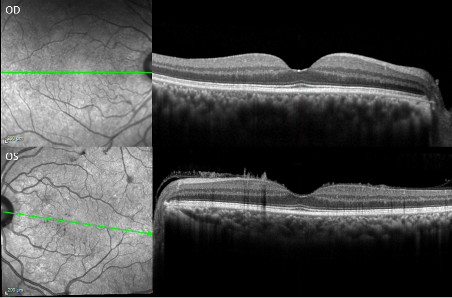
Optical coherence tomography of macula of both eyes. The left eye reveals needle-shaped deposits on the anterior retinal surface extending into the vitreous.
DIFFERENTIAL DIAGNOSIS
- Most suspicious for amyloidosis given long history of symptoms, glass wool-like anterior vitreous opacities, white perivascular deposits seen on fundoscopy, and needle-shaped deposits along the anterior retinal surface on OCT
- A broad differential may also include the following:
- Infectious: syphilis, tuberculosis, toxoplasmosis, endophthalmitis, Lyme disease, Whipple’s disease
- Inflammatory: sarcoidosis, multiple sclerosis
- Neoplastic: lymphoma, leukemia, metastatic disease
WORK UP
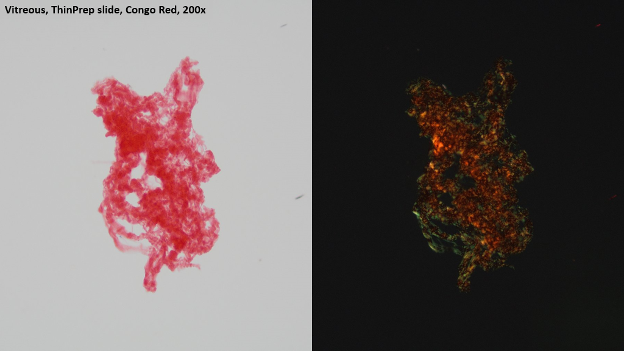
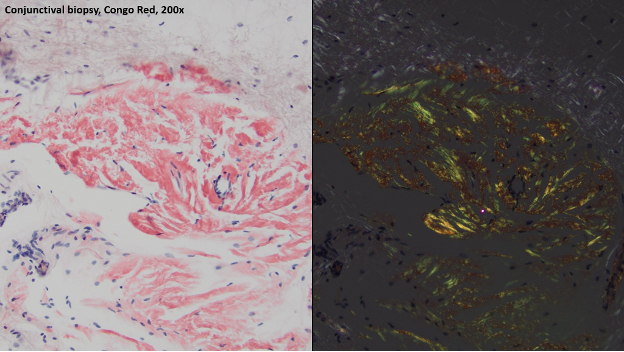
- S/p PPV OS with vitreous and conjunctival biopsy sent for Congo red stain. Of note, the vitreous was found to be remarkably adherent, and the hyaloid was not able to be lifted at the time of this surgery.
PATHOLOGY SLIDES
Pathology slides of the vitreous and conjunctiva with Congo red stain demonstrating apple-green birefringence, consistent with amyloid deposit.
FURTHER MANAGEMENT
- S/p repeat PPV (to lift the hyaloid) and GDD placement OS for mixed mechanism glaucoma (secondary glaucoma related to amyloidosis and steroid use)
- Genetic testing revealed a mutation in the TTR gene
- Referral for systemic evaluation – found to have cardiac amyloidosis and amyloid-related polyneuropathy
- S/p CEIOL OS
- Pending CEIOL OD
- Recent BCVA 20/40 OU, IOP 21 OD, 9 OS on dorzolamide and timolol BID OU
DISCUSSION
- Amyloidosis is a potentially fatal group of diseases characterized by the deposition of misfolded proteins within various organs.
- Ocular involvement in amyloidosis depends on the subtype of disease, most commonly seen in light-chain amyloidosis.
- Protein deposits can be seen in many tissues in and around the eye, but a few classic findings for the vitreoretinal surgeon to look out for include “glass wool” appearance of the vitreous, white perivascular deposits seen on fundoscopy, and needle-shaped deposits along the anterior retinal surface seen on OCT.
- Other ocular complications, such as amyloidosis-related glaucoma, are common and may require intervention.
- Congo red staining of a vitreous sample may reveal the protein deposits with apple green birefringence.
- The vitreous serves as a scaffold for protein deposition, so PPV is the treatment of choice for visual rehabilitation in these cases.
- Relapsing vitreous amyloidosis may require repeat PPV.
- This is a potentially fatal disease, and prompt referral for systemic evaluation is critical.
- Ocular disease can progress even after some systemic treatments, so continued follow up is important.